Dealing With Chronic Pain And Fatigue

I AM SO TIRED…
Mike’s name was called three times in the waiting room by the office staff. No one waiting responded. The office manager saw a man asleep in the corner chair (one of the soft sofas) and went over to him, “Excuse me sir, is your name Mike?” He opened his eyes, smiled, and followed her back into the examining room.
“Doc, I am so tired that I don’t want to get out of bed. I lost my job…my wife is frustrated with me…and we are about to lose our house in foreclosure. I have pain all the time and my Primary Care Physician (PCP) told me I just have to live with my pain. How am I to do that?”
Mike is one of many people seen in clinical pain management practices dealing with chronic pain and fatigue. This complication of chronic pain is often over-looked by PCP’s as they have so little time and so much to do for their patients these days.
WHY…
When a person suffers from the Chronic Pain Syndrome (click here to link to it) they will often develop an overwhelming fatigue syndrome in addition to their pain. This can be a signal that they have begun to enter into the negative neurophysiologic changes that accompany the Chronic Pain Syndrome.
Nearly all neurotransmitter production in the central and peripheral nervous system has a fixed maximal production capacity.
Continual electrical stimulation from chronic pain “outstrips” the production capacity of the neurons. When this happens secondary symptoms begin to occur…depression, insomnia…fatigue…etc..
The usual approach many Doctors use is to treat these secondary symptoms as a separate illness. This only stresses the neurons further.
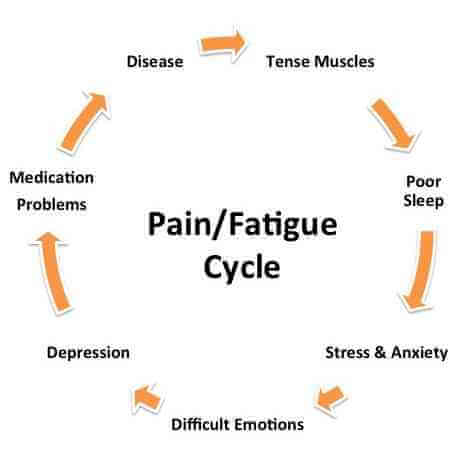
It is akin to “whipping a horse” when it is exhausted…the horse may die before it gets to the finish line. A more physiologic approach would be to decrease the neurotransmitter “drain” and restore the supply.
WHAT CAN I DO…
The most physiologic approach to the management of chronic pain and fatigue would be as follows (this regimen, as described, would be approved and administered by a licensed medical practitioner. The information contained in this blog post is not to be construed as medical recommendations):
A) Step 1: Reduce or eliminate the “drain” of neurotransmitters that is occuring. That may be accomplished in the following way:
1) Effectively treat a persons’s pain. Most people who have deteriorated to the point that they are developing secondary symptoms from chronic pain can give you an estimate of what their pain medication needs would be.
A Doctor can use their history of pain medicine effect to guide them as to what the starting dose of prescription pain medication could be.
2) Establish what the sleep pattern of the person is. Sleep deprivation in chronic pain patients is very common (click here to see my article on “The Sleep disorder In Chronic Pain”) . When properly medicated for pain they will often have what is called “REM rebound” (they may sleep 2 or 3 times the length they usually would).
Click edit This does not mean they are over-medicated. They are “catching up” on their sleep. They are, in effect, resupplying their neurotransmitters. This period of time is often misinterpreted by Doctors and family alike.to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
3) A non-sedating anti-depressant in low doses may be started (preferably one that “recycles” both norepinephrine and serotonin). An example of this would be a medication called Cymbalta.
4) It may be necessary to start a low dose sleep medicine, in the early phases of restoring the neurotransmitters, to initiate a more normal sleep pattern. The objective would be to use this short-term.
5) It may also be necessary to use a low dose neuro-stimulant to “push” the neurons so that the person will be functional enough to return to work. The objective of this medication is also to be used short-term.
B) Step 2: Gradually replenish the levels of neurotransmitters in the central and peripheral nervous system. This may be accomplished by:
1) Consider the nutraceutical regimen that was described in my blog post on Fibromyalgia (click here to link to it).
2) Begin a gradual exercise program beginning with water based (low gravity effect) exercise gradually increasing to land based exercise. The program would be best focused on building endurance gradually (this increases the number of energy generating organelles called mitochodria).
3) Have a Consultation with an expert in Complementary and Alternative Medicine (CAM). They will be able to fashion a nutraceutical and dietary regimen to enhance energy production.
4) Have Phases 1 and 2 carefully supervised by your PCP.
THERE IS HOPE…
Mike went on to do well. He was able to follow many of the recommendations that were offered to him. Over a period of 12 months he returned to work and was able to keep his home. He even took a second job for a period of time until his finances stabilized.
If you are suffering as Mike did there is hope. You need to call your PCP and get started on your way to recovery.
Please leave an e-mail and tell me your story. I would love to be of service to you ([email protected]).
Facebook
Google+
Twitter
Pinterest
Reddit
StumbleUpon