Laminectomy, Discectomy and Microdiscectomy

Surgical Treatments
Spinal surgery may be an important aspect not only of pain management, but also in restoring neurologic or biomechanical stability. However, just as spinal surgery may ameliorate symptoms in patients with low back pain or related conditions, spinal surgery also may worsen symptoms. Some patients have multiple failed interventions, only to have another failed surgery in an attempt to rectify the pain. Two conditions necessitate performing immediate lumbar spine surgery:
- Loss of bowel control, bladder control, or both as a result of the lumbar spine condition.
- Rapidly progressive or absolute muscle weakness as a result of the low back condition.
A relative indication for low back surgery is that the patient has failed good, nonsurgical management for treatment of his low back condition, and the patient is presenting with a well-defined, anatomic basis as a cause of low back pain. As discussed earlier, it is more often the case that pain is driven by both anatomic and physiological factors. However, an astute clinician can discern when pain is primarily the result of an anatomic malfunction.
Medical Risks of Surgery
Before a patient can be considered for surgery, an internist or primary care physician and an anesthesiologist must assess the medical risks of surgery. Most lumbar spine surgery involves placing the patient under general anesthesia. This is a coma-like state in which the patient is intubated , which means that a ventilator is performing the action of breathing for the patient. While the patient is in this coma-like state, surgery can be performed painlessly, and the anesthesiologist monitors vital signs such as blood pressure and heartbeat.
General anesthesia and recovery from surgery place an extra stress on the heart. Therefore, the treating physicians must account for any possible weakness of the heart muscle or any possible blockage of the coronary arteries that supply blood to the heart muscle. Often, patients undergo special heart tests such as an exercise stress test and echocardiogram before they are cleared for surgery.
General anesthesia and recovery from surgery also stress the lungs. The lungs have a natural tendency to expand incompletely following surgery. In addition, because of pain following surgery, patients may be reluctant to take full, deep breaths. If the lungs do not expand fully with good deep breaths after surgery, then there is a risk of developing an infection or pneumonia following surgery. In patients who have compromised lung function to begin with—for example, chronic bronchitis or chronic obstructive pulmonary disease—then the risk of developing pneumonia or other lung problems increases, thus complicating surgery.
Some patients have other medical problems, such as diabetes and high blood pressure. General anesthesia and surgery can cause these medical conditions to worsen, especially following surgery, when the body is struggling to recover. Thus, all treating physicians must pay careful attention to monitoring and properly treating such conditions during and after surgery. Infection may develop following any surgery, and is more common in more complicated surgeries such as spinal fusion.
In essence, general anesthesia, surgery, and recovery from surgery place tremendous stress on the body in general, and the heart and lungs in particular. Younger, healthier patients generally have no difficulty tolerating such a procedure. However, medically ill or elderly patients deserve special consideration before they are cleared medically to undergo surgery, and they require intense monitoring following surgery.
Laminectomy and Laminotomy
Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

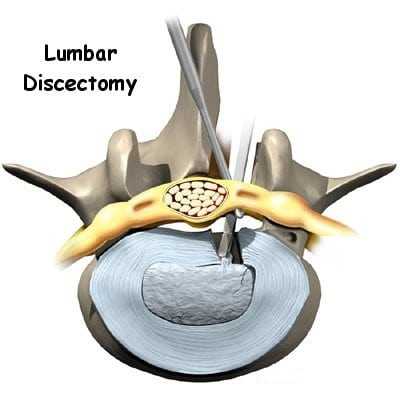
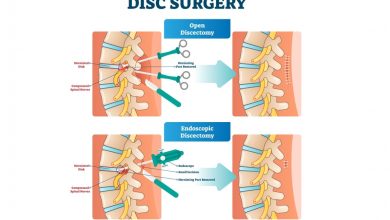
Laminectomy means that the lamina, which is part of the normally non-weight-bearing part of the lumbar spine, is partially cut so that the spinal surgeon (orthopedic surgeon or neurosurgeon) can view the contents of the spinal canal (Image 1). Typically, just one side of the lamina is removed. However, if the surgeon requires more operating space, both sides of the lamina plus the posterior spinous process are removed (Image 2). Following removal of part of the lamina, the surgeon can remove a fragment of a herniated disc or can perform techniques to widen the spinal canal, as is necessary in lumbar stenosis. (Lumbar stenosis, which is discussed in article, is a degenerative condition of the spine that results in spinal canal narrowing.)
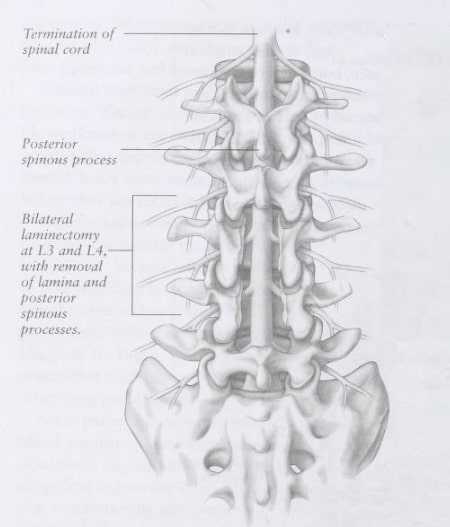
Sometimes, a laminectomy is performed at more than one level (Image 2). For example, a patient may present with two or more levels of disc herniation or lumbar stenosis that require surgery. Even though laminectomies can be performed at multiple levels, as the number of spinal joints affected increases, there is an increased risk for developing spinal instability following such surgery. Spinal instability means that the vertebrae no longer move in a properly coordinated manner. Rather, the vertebrae may slip forward or backward with body position changes. This slippage can cause pain and, when severe, can lead to nerve irritation or nerve damage.
Laminotomy means that a hole is drilled through part of the lamina. Laminotomies are performed when the surgeon requires only a small viewing area to perform surgery (Image 1).
Recovery from laminectomy or laminotomy is generally within days. The patient may be discharged from the hospital within 1 or 2 days, and is walking immediately. Physical rehabilitation begins within a few weeks of the procedure. As with any surgical procedure, a risk of infection follows laminectomy or laminotomy, although the risk is small. Nerve damage is rare. The biggest risk is that the patient must undergo general anesthesia and must be medically fit to do so.
Discectomy and Microdiscectomy
Discectomy simply means that part of the lumbar disc is removed. Unless a spinal fusion procedure is performed, most diskectomies are done as part of a laminectomy or laminotomy. The purpose of the procedure is to remove that part of the disc that is placing pressure on a nerve or other pain-sensitive structure. The rest of the disc is left in place (Image 3).
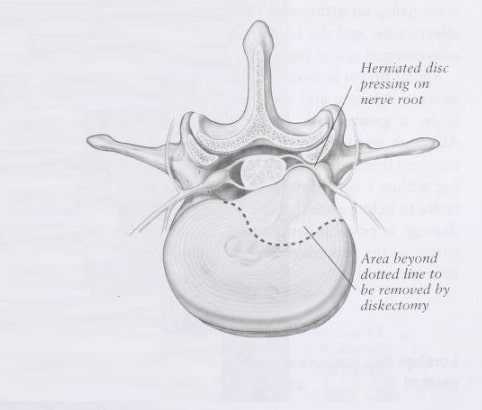
Image 3 – Discectomy
Microdiscectomy means that the entire surgical procedure is performed through a smaller incision, because the surgeon utilizes a microscope for the purpose of magnification. Discectomy and microdiscectomy are appropriate procedures for herniated lumbar discs that are the primary anatomic basis of the patient’s pain. An alternative to microdiscectomy is percutaneuos lumbar discectomy, in which the surgery is performed through a small arthroscopic port; this procedure is less well-studied than microdiscectomy. The risks of discectomy and microdiscectomy are similar to those of laminectomy.