Pain after Back Surgery

It is not uncommon for patients to develop some pain after back surgery even if they initially experience significant pain relief. The reason for this remains largely unknown with some claiming that scar tissue is responsible for the nerve pain, and others observing that patients whose MRIs reveal similar scar tissue do not experience this pain. If pain comes on gradually after back surgery then it may, indeed, be the formation of scar tissue that is causing the progressive condition. Acute pain in the leg or back is more likely attributable to a herniated disc due to spinal instability or poor preoperative diagnosis. Recurrent pain after six months or more is not likely to be solely attributable to the scar tissue from back surgery, but this fibrosis may be responsible, in part, for a more rapid progression of symptoms from spinal stenosis due to osteophyte growth or disc herniation.

Other considerations include the failure of the surgery to remove all of the material compressing the nerve, the growth of new bone spurs which pinch the nerve, hardware failure or movement, infection in the deep tissues and bone, dural tear, failed fusion, spinal slippage, and deferred pressure on adjacent segments. It is also possible that the nerve damage prior to surgery was simply too advanced and the patient achieves no substantial pain or symptom relief following back surgery. Treatment for pain after back surgery depends largely on the cause of the pain, assuming it can be established. Physical therapy and pain medication is the usual therapy, with surgery to remove scar tissue rarely performed due to the risk of further scarring and the difficulty in confirming the scarring as the cause of the pain.
Patients are encouraged to follow post-surgical guidelines closely in order to minimize the risk of problematic scar tissue formation. Extended periods of inactivity can allow the scar tissue to form over a nerve root and ‘tether’ it in such a fashion that pinched nerve symptoms arise once again. Conversely, returning to work and physical activity too quickly may encourage an inflammatory reaction and fibrosis. Restrictions on heavy lifting, twisting, and bending are usually put in place for a certain period after back surgery, with guidance varying according the extent of the procedure. Patients undergoing minimally invasive X-Stop procedure, for example, are likely to return to normal activities in a much shorter period than those undergoing a discectomy with laminectomy and spinal fusion.
Whilst some patients may simply experience a continuation of the symptoms they had prior to back surgery, some will experience novel symptoms that require investigation. If a patient develops new symptoms of back pain or leg pain after back surgery then a full physical examination, combined with diagnostic imaging, is indicated. This may identify the cause of the patients’ pain, but may, in some cases, reveal no clear pathology at work. For a number of patients the MRI or X-Ray will reveal problems with hardware used during spinal fusion surgery. For others there may be indications of a disc herniation or disc bulge at a different level to that operated on.

Recurrent Disc Herniation
In cases where an initial period of pain relief after back surgery, such as a discectomy, is followed by acute pain in the back or leg there may be reason to suspect recurrent disc herniation. Where symptomatic pain is due to fibrosis (scar tissue), the symptoms tend to appear gradually rather than acutely. It is important that patients follow post-surgical guidance to reduce the risk of recurrent herniation. Advice is likely to include staying hydrated following surgery as dry discs can become brittle and rupture more easily, and avoiding twisting, bending, or lifting to varying extents in order to reduce stress on the intervertebral discs, at least during the recovery period.
If a discectomy was performed, with a laminectomy, and/or spinal fusion, the segments of the spine adjacent to the operative level may have been put under extra pressure and the speed of disc degeneration can be increased. The intervertebral disc may bulge or rupture causing a pinched nerve and the resulting sciatica or other nerve pain. Patients with a history of disc problems are more likely to suffer from recurrent disc herniation and an MRI should be able to identify this as the cause of their symptoms.
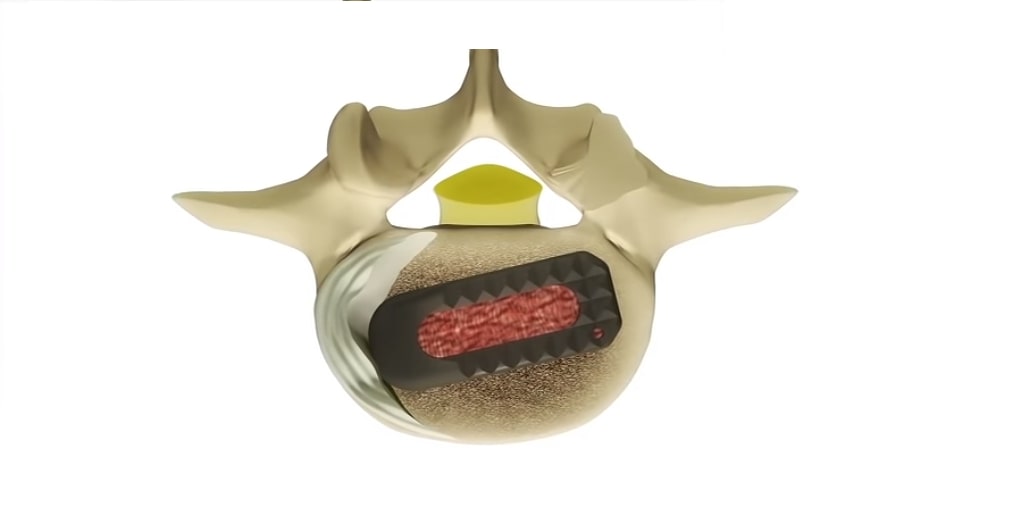
A number of treatment strategies are available to address the problem, with patients usually given a conservative treatment plan for a number of months including physical therapy, NSAIDs, epidural steroid injections, or other therapies. In cases where symptoms progress rapidly with the occurrence of bowel/bladder incontinence, significant weakness in the legs, or persistent pain which fails to respond to medication, the patient may require further back surgery to achieve decompression. This surgery may be more extensive and involve the use of spinal fusion to stabilize the spine. The use of the TLIF surgery may help prevent recurrent disc herniation as this restores and maintains the intervertebral height and relieves some of the pressure that may otherwise be placed on adjacent segments following discectomy.
Use of the X-Stop device to relieve symptoms of spinal stenosis such as sciatica may only be helpful for a short period if spinal degeneration continues to progress. Whilst this device can effectively relieve sciatica symptoms stemming from the lumbar spine it will be largely ineffective if the symptoms are actually due to piriformis syndrome where the sciatic nerve is impinged by the thigh muscle. Accurate diagnosis is clearly of paramount importance in order to reduce the risk of unnecessary back surgery. As the X-Stop is usually only implanted at one or two surgical levels it is inappropriate where patients have stenosis and disc degeneration at multiple levels.
Back or leg pain that occurs several months after X-Stop surgery is usually not attributed to the device itself, with other spinal conditions implicated instead. Back pain that occurs quickly after implantation of the X-Stop may be due to fracturing of the spinous process, movement of the device after surgery, or incorrect positioning by the surgeon. Although patients should be assessed carefully prior to X-Stop surgery to ensure that no anatomical variation would prevent the procedure being carried out, surgeons should always halt the operation if, upon accessing the back of the spine, they discover that the patients’ anatomy is likely to affect the device’s correct function.
Preoperative Patient Selection for Back Surgery
One of the most common causes of failed back surgery syndrome and recurrent pain after back surgery is the poor diagnosis and selection of patients as regards the spinal pathology at work. Whilst diagnostic imaging can help a clinician highlight a likely troublesome lesion or structure in the spine, there is no guarantee that it is this particular anatomical variation that is responsible for the patients’ symptoms. The use of selective nerve-root blocks prior to surgery can help relieve the patients’ pain and clarify which nerve is the cause of the symptoms of back pain, leg pain, numbness, weakness, and paraesthesia.
Some lesions in the spine are more reliable than others as predictors of back pain, with a disc herniation more likely to be the root cause of leg pain than it is of back pain, for example. Accurately diagnosing piriformis syndrome as the cause of sciatica symptoms can save a patient from undergoing unnecessary back surgery, and sacroiliac joint dysfunction (common amongst regular golfers) may be responsible for lower back pain and leg pain. Although certain misdiagnoses are unlikely, osteoarthritis or rheumatoid arthritis could be overlooked if a clinician finds initial evidence of spinal lesions and stenosis which could be the cause of back and leg pain.

Surgical Error or Complication of Back Surgery
In any back surgery procedure there is a risk of technical error and the development of back pain, leg pain, and other symptoms during the recovery period. Some surgeries are more risky than others, with traditional open laminectomy with fusion liable to cause significant muscle, and ligament trauma and increase the possibility of scar tissue formation. Conversely, minimally invasive surgeries usually reduce the risk of nerve and tissue trauma and are considered less likely to result in pain development after surgery. New techniques do require the surgeon to be particularly skilled in using an endoscope and specialized surgical instruments however, and the often tiny surgical field can present a narrower margin for error.
When operating very close to the spinal nerves, such as during a foraminotomy, discectomy, or TLIF procedure, the surgeon must remain cautious at all times as regards the potential for nerve trauma. Retracting the nerves to keep them out of harm’s way during the procedure can itself cause bruising to the nerve and a degree of pain after surgery as the nerve heals. It is possible that the nerve be cut due to surgical error during back surgery, and this may cause pain, weakness, or even paralysis. Severance of spinal nerves is, however, extremely rare during back surgery.

Patients may suffer a dural tear during surgery which is where the surgeon accidentally nicks the membrane covering the spinal cord. Procedures such as the X-Stop do not carry this risk as they are performed outside of the spinal canal, but more invasive procedures to removed discs, perform fusion, or clear osteophyte growth may result in a surgical slip. In the majority of cases this is noticed at the time and the surgeon can repair the tear with little risk of complication after surgery. If, however, the dural tear goes unnoticed then the patient may experience a seepage of spinal fluid and the possibility of infection. The infection may spread to the meninges and cause spinal meningitis, a potentially fatal condition. Headaches, stiffness, fever, and swelling are warning signs for infection and should be reported immediately for investigation.

Patients will usually feel a slight amount of pain at the incision site after back surgery and the area will be a little sore and red. However, extreme pain, swelling, and redness that extends beyond a centimeter or so from the incision line may indicate infection. Some surgeons offer prophylactic antibiotics to reduce the risk of infection after surgery, and shallow, superficial, infection will usually clear up with antibiotic use. In the case of deeper infection, in the bone or other tissues of the spine, the patient may need to undergo further surgery to remove infected tissue and drain the infection. Scar tissue after back surgery following infection may lead to an increased risk of postoperative back pain and leg pain.
A further consideration is the possibility that the back surgery failed to remove all of the material causing nerve compression leaving, for example, fragments of disc material, bone spurs, or calcified ligament which could result in continued or developing nerve pain. This will usually mean that the patient achieves little relief from the procedure with the potential for the pain to worsen over time. The presence of pain immediately after surgery contrast with the gradual pain progression usually indicative of scar tissue pathology. Further surgery may be required to remove the residual material. Some minimally invasive back surgery, such as laminotomy or laminoplasty may increase the risk of incomplete spinal decompression due to the restricted visual field available to the surgeon. The use of a fluoroscope during surgery can aid their appraisal of the degree of decompression achieved and is often incorporated into surgeons’ best practice guidelines.