Spinal Stenosis and Sciatica
Stenosis means narrowing. To understand spinal stenosis, it’s necessary to make the distinction between two types of openings: one in the neuroforamina and the other in the spinal canal itself. The neuroforamina are the little openings between the vertebrae at which the nerve rootlets consolidate into roots and through which they exit the spine like the branches of a Christmas tree leaving the trunk—symmetrically on both sides. The fibers in those nerve roots arc destined to descend to the lumbosacral plexus, where they combine, divide, and recombine to form the peripheral nerves, including the sciatic nerve. When these little neuroforaminal openings are narrowed because of swelling, irritation, or some other problem, the result is a radiculopathy: pain And possibly sciatica, but not spinal stenosis. For example, it the nerve roots that come out of the neuroforamina at L4- L5 are compressed because they don’t have enough space, you will feel it on the skin inside your calf, and the ability to lift your foot at your ankle will be compromised as a specific consequence of injury to a specific nerve root.
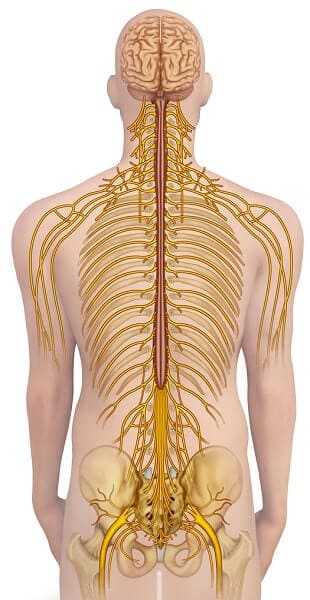
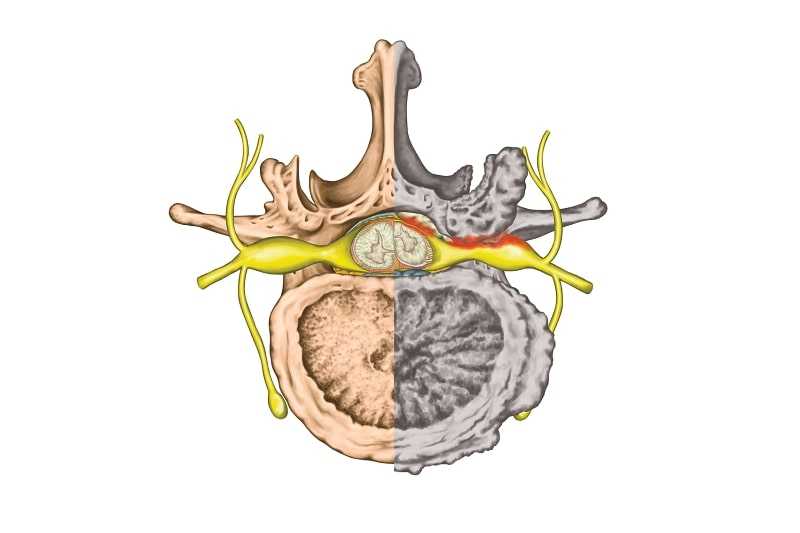
Spinal stenosis is narrowing within the spinal canal itself. If that happens and you have compression at the same level that 1 described above, it could affect the same nerves with the same feelings, the same weaknesses. After all, the same nerve fibers are involved; it’s just that they’re injured at a slightly different place. But there’s a distinction. If the problem is in the neurotoramen, it’s just one nerve that is injured. But if it’s the central canal, it could easily affect nerves on both sides below it, at L5-S1 and any and all nerves below that. That’s a big difference. The symptoms may be different. When you have a single level at which an injury occurs, you have a neat package of symptoms that many physicians can recognize at once, and identify. Recognizing spinal stenosis may be a challenge.
Symptoms, Diagnosis, and Causes
Stenosis often begins with a vague kind of discomfort over broad areas o{ skin, even in places that are not related to the sciatic nerve. You may feel numbness or tingling, mild or severe burning sensations at the outside of your thighs or in your calves or feet. Unlike problems with the neuroforamina, symptoms of stenosis are often bilateral—more or less symmetrical, though that doesn’t mean they’re always or necessarily exactly equal on both sides. Some cases of stenosis are evident on one side only. Stenosis can have a number of different manifestations. You may feel it on the inside of the arches of your feet, or inside the thighs, or just below the buttocks or knees, or a combination of these.

The reason the symptoms may be hard to pin down is that swelling inside the spine is usually (but not always) progressive, and the narrowing is often a chronic and incremental process. The progression isn’t smooth or linear. Today you may experience mild pain, another day it feels as though you’re wearing sweat pants even though you may be wearing nothing. When stenosis is sudden, it can come from a disk that has begun to bulge or has cracked and become swollen in the middle of the spine, instead of nearer the outer edge, where it is at the neuroforamen. Nevertheless, the swelling that results may mildly compress one clump of rootlets today and another clump a week from now.
A significant feature of stenosis is that the symptoms are often worse when the spine is straight. That means you will be more uncomfortable when you’re lying flat and are horizontal, or standing up and entirely vertical. Sitting with the spine somewhat curved provides some relief, as does lying in the fetal position. A simple explanation for this is that nerves are stretched more and are therefore thinner when the spine is curved. When your spine is straight, the nerves are as thick as they can get in a space that doesn’t enlarge, and therefore they are more subject to compression.
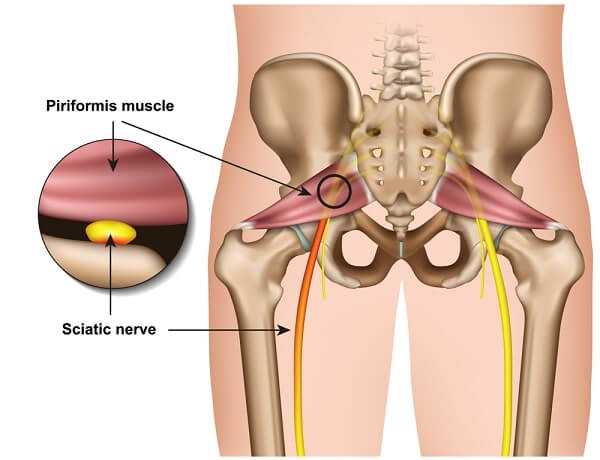
If there is sciatica, but the symptoms don’t fit into a neat package of a single level of spinal injury, that’s another suggestion that you might have stenosis. There are ways to distinguish this problem from piriformis syndrome. First, piriformis syndrome is almost always worse when you’re sitting down. Second, in spinal stenosis, pressing the buttock is painless. If there are symptoms or signs in the front of the thigh, or the inner part of the calves, it’s due to an injury of fibers that are not part of the sciatic nerve. These never come close to the piriformis muscle, so piriformis syndrome is not the problem in this case.
Stenosis often distinguishes itself from most radiculopathies because pain doesn’t occur at a specific place or have an abrupt beginning, and there is pain on both sides. Unlike a disk problem at the neuroforamen, this condition can interfere with all the nerve rootlets of the cauda equina below it. The nerves that control the sphincters of the bowel and bladder can be affected. If you feel ascending numbness or weakness, or if you have issues with bowel and bladder control, that is a medical emergency and requires immediate attention. Very unusual, sudden, and severe lumbar spinal stenosis can cause cauda equina syndrome, and limit voluntary control of all muscles and sphincters below it.
To be absolutely certain that your problem is stenosis, you will need an MRI. This diagnostic test can determine the size of the space inside the spinal canal and can outline the soft tissue inside it, such as the ligamentum flavum and the nerves. The EMG is the gold standard of measuring how much damage there is, and at what levels it has occurred. A myelogram or the injection of X-ray contrast fluid by a radiologist is also useful in showing the exact location and nature of any compression. It is done in conjunction with an X-ray or CT scan, often before surgery is performed.
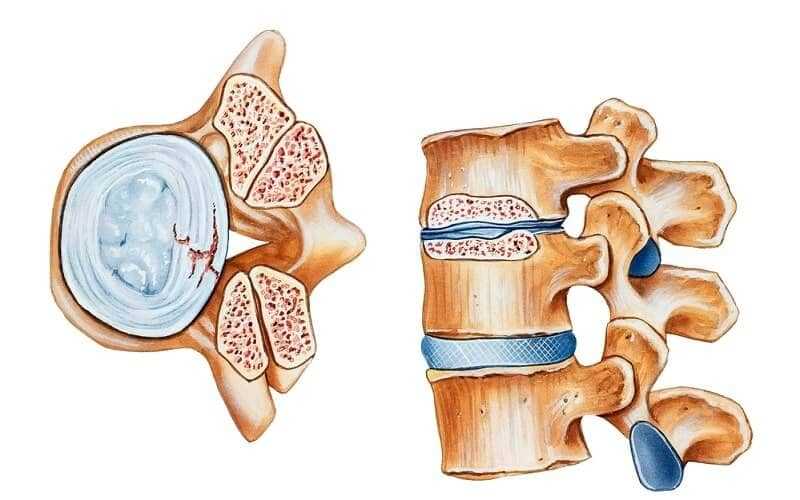
Spinal stenosis most often results from a gradual, degenerative aging process, but not always. Three elements precipitate this condition. A cross section of the spinal column at any level from the top to the bottom always contains the same elements: the bony sides of the canal; the disks, which separate the vertebral bodies at the front of the canal; and the ligamentum flavum (the yellow ligament), which lines the back of the canal continuously from the neck down. Stenosis comes about when one or more of these elements bulges or herniates into the canal, narrowing it enough to put pressure on the nerve fibers within it.
This reduced diameter occurs most often and predictably when osteoarthritis and similar processes thicken the bones. When you’re young, your bones get longer; with age, they get thicker, and the spaces within the bone become narrower. (See illustration on below.)
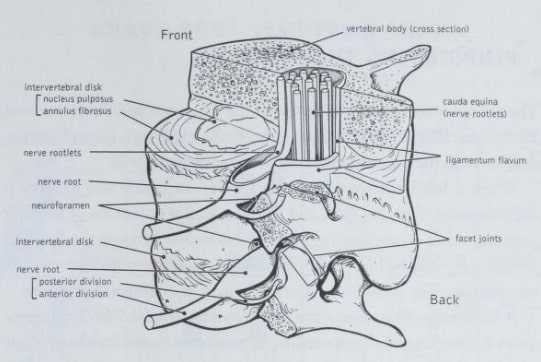
If the ligamentum flavum thickens, the space available for the nervous tissue is decreased by the same amount. Although age and chronic, gradual processes such as osteoarthritis are generally responsible for bony thickening, it is an abrupt event or a short-term situation such as sleeping in an unnatural position on a cramped couch for a couple of hours that can cause the ligamentum flavum to swell and constrict the available space.
Disks bulge and herniate for all kinds of reasons—from lifting firewood and reaching for the turkey platter while serving a large gathering, to falls, overuse, and awkward movements in restless sleep. Whereas the bony changes and ligamentum flavum thickening can occur throughout a large sector of the spine, disk-related narrowing is usually located at one particular level.
The illustration on above makes it clear that a significant enlargement in any oi these three elements is no more serious than mild or moderate enlargement in two or three of them. Yet the remedies for the three are quite different. We’ll get to that later. For now, we’ve characterized spinal stenosis, and gotten familiar with its causes.
When spinal stenosis produces pain, it’s rarely explained by a single acute event. Various elements limit the space inside the spinal canal, and something happens to disturb the normal equilibrium of two of the following three elements:
* the ligamentum flavum, which stretches continuously from the neck to the sacral spine
* the disk that abuts on the cylinder at each level
* the actual diameter of the cylinder that the nerves pass through
Treatments for these situations are different. If the ligamentum flavum has become swollen, usually steroids introduced into the epidural space will reduce that swelling— until you sleep on that short couch again or do whatever you did to bring about the pain. Steroids may cure your condition forever. If it’s a disk problem, steroids can be helpful here, too, in reducing the size of the disk itself and damping down the chemical reactions that often ensue from its inflammation. And that will also provide more room for the nerves. If the cause of the stenosis is due to changes in the bones, surgery is the only reliable cure. There is an exception to this, however. If you’re in an acute situation, epidurals may work by narrowing other elements and reducing inflammation that the narrowing of bone has produced, at least for a few weeks. You can often buy a little time with epidural steroids.

How do you determine the cause of any particular case of stenosis? An MRI is invaluable. Neuroimaging may prove to be valuable, and in the future such techniques may be able to reveal the exact nature of an injury. Your medical history and a complete physical will also be helpful. If the condition has an abrupt onset, chances are it’s not just osteoarthritis and the slow and inevitable encroachment of thickening bone into the spinal canal, but specific events that have produced bulging or herniation of a disk or swelling of the ligamentum flavum. Steroids are more likely to work in an acute event than with chronic, creeping, encroaching bone. If the symptoms are gradually increasing, if they involve the outside of your thighs, going down toward your knees and lower part of the legs, you have a chronic, progressive problem. Rather than drift into the position of an old person whose cardiovascular system will no longer tolerate an operation, without which life is either unbearable or dominated by having to take many medications, surgery is the most sensible alternative.