TLIF – Transforaminal lumbar interbody fusion
Spinal fusion may be recommended for many patients with a variety of spine conditions. A few of the conditions that cause mechanical pain in the back and neck where a fusion is considered are:
- Spondylolisthesis
- Herniated Disc
- Degenerative disc disease
- Spinal stenosis
The transforaminal lumbar interbody fusion (TLIF) technique is just one of the options that a spine surgeon may consider in order to stabilize the lumbar spine and try to prevent pain from curvature, slippage, hypermobility, or stenosis.
What is a TLIF?
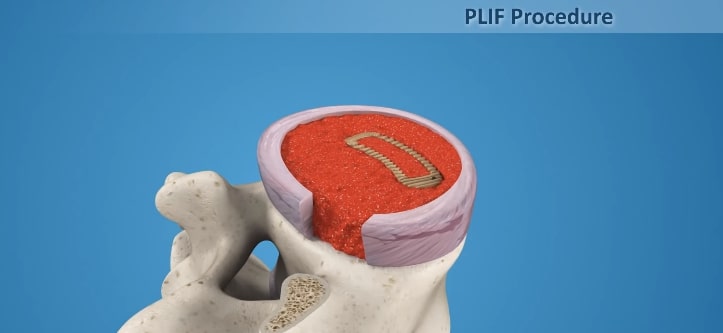
TLIF is a kind of spinal fusion where the surgeon positions an implant between the problem vertebrae in order to fuse these vertebrae together and eliminate painful segmental motion in the spine. This procedure is minimally invasive in comparison to the conventional PLIF technique which causes more muscle damage and blood loss, often requiring transfusion. Patients are usually able to stand and walk the day after TLIF, whereas PLIF surgery necessitates prolonged bed rest. Recovery is shorter and allows patients to return to work (with some restrictions) after a matter of weeks rather than months.
The TLIF Procedure
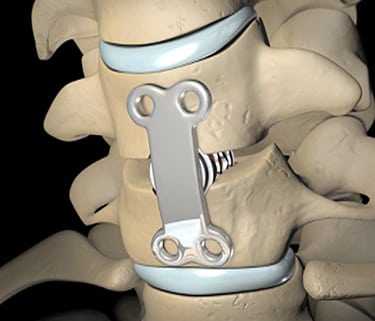
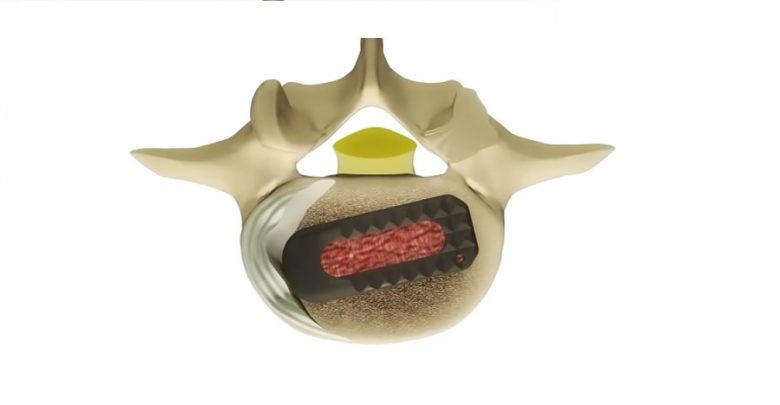
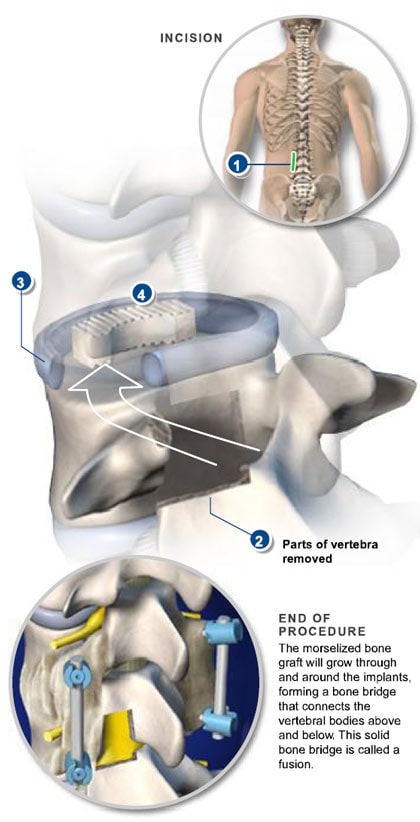
TLIF is performed through an incision in the posterior of the spine, from a lateral approach and requires the removal of the facet joint on one side to access the disc space. Surgical hardware (instrumentation) is used to enhance the chances of successful fusion occurring with an interbody spacer positioned between the vertebrae in the disc space to restore and maintain intervertebral height and reduce stenosis symptoms. A bone graft (either an allograft or autograft) is inserted to facilitate fusion, and pedicle screws and rods are used to connect the two, or more, vertebrae at the back. TLIF forms a fusion between the anterior and posterior of the spine using only a posterior lateral approach, making this a preferred back surgery for many in contrast to operations requiring both an anterior and posterior approach or more invasive access from both sides of the posterior spine (PLIF).
TLIF Facts
The use of an interbody spacer allows intervertebral height to be restored and pressure to be taken off the nerves. Bone fusion is often enhanced using this procedure as both the interbody bone graft and the posterior bone graft form a solid, stable, structure to reduce spinal segmental motion. In TLIF surgery the interbody spacer and bone graft are put into position using a lateral (side) approach which can reduce the incidence of nerve trauma and scarring compared to a posterior lumbar interbody fusion (PLIF) procedure. The success rate for relieving pain after TLIF is around 60-70%, with the majority of patients satisfied with surgical results. Risks with TLIF include all the usual surgical risks of infection, blood loss, problems with the anaesthetic, and scarring. TLIF does reduce the risk of nerve trauma (compared to PLIF) but still holds some potential for altered nerve function such as numbness, pain, weakness, and paralysis. It is also possible that the fusion will not be successful and non-union occurs, leading to the possibility of further surgery or persistent pain. Fusion of the spine also carries the risk or deferring stress and strain onto other spinal segments leading to a higher propensity for degeneration, fracture, and pathology at these segments.
Patients Considering a TLIF
Patients considering back surgery using a TLIF procedure will usually be asked to quit smoking prior to surgery as this can significantly reduce the chances of a successful fusion. The pre-donation of blood is usually unnecessary with this minimally invasive back surgery. Patients with disabling back and leg pain are likely to achieve some degree of relief from this procedure but should be aware that in some cases the extent of pre-existing nerve damage will preclude a full recovery. Discussing expectations of outcome with the physician prior to surgery will help reduce disappointment if poor results are experienced. Conservative treatments such as physical therapy, medications (NSAIDs, and epidural steroid injections), and alternative treatments like acupuncture, chiropractic, massage, and yoga, may be helpful and postpone or remove the need for back surgery and are usually utilized for six month or so prior to surgery being considered.