Acute Disc Herniation Treatment
Non-Surgical Treatment
Activity: Bed rest is not recommended but in extreme cases may be required to overcome the initial pain. Beyond 48 hours, however, bed rest becomes detrimental to recovery and should not be encouraged.
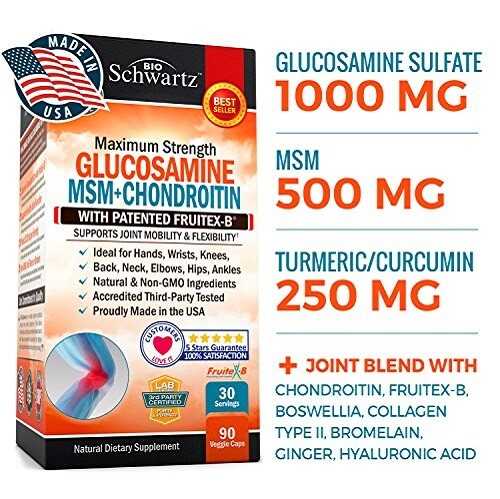
Medications and Supplements: Immediate use of analgesics (including cautious use of narcotics) and anti-inflammatory medication is valuable to reduce pain and allow improved mobility. The use of muscle relaxants remains controversial. Pain-relieving anti-depressant medication such as amitriptyline can be used judiciously. Valuable supplements include essential fatty acids (for example, flaxseed oil), B-vitamins (particularly B-12) for nerve recovery, manganese, glucosamine sulphate and MSM for the disc, and arnica and ginger for inflammation. Physical modalities such as heat or ice may reduce discomfort, as will TENS and acupuncture.

Posture: Finding a comfortable posture involves a little experimentation. Lying with a roll under your low back to increase extension and supporting the affected leg in a flexed hip and knee position may work. Others find lying on their front with a pillow underneath the pelvis or arched back supported on the elbows beneficial. Periods of activity followed by shorter periods of rest reduce discomfort and maintain a certain level of activity and function.

Exercise: Exercises are difficult due to pain, at least during the first few days. However, a back extension program including the “sloppy-push-up” is useful to reduce pain and restore mobility. Flexion exercises should be avoided.
Traction: Traction is reported to be useful in reducing herniations and nerve compression but this is not born out by clinical study.
Contraindications: Chiropractic and massage therapy are not recommended during the acute phase.
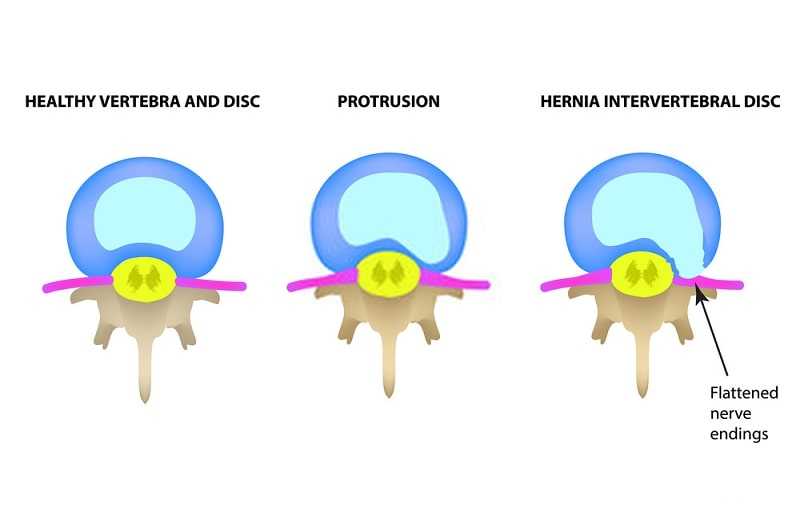
Acute Disc Herniation Facts
In the absence of any ‘Red Flags’, initial management of acute disc herniation is non- surgical.
Recommended Non- Surgical Treatments
• Heat
– May reduce spasm/pain
• Acupuncture
• Medications – Analgesics and Anti-inflammatories
– Cautious Use of Narcotics
– Tricyclic Anti- Depressants (for pain)
• Natural Supplements
– Essential Fatty Acids
– B-Vitamins (particularly B-12)
– Manganese
– Glucosamine Sulphate and MSM
– Arnica, Ginger
• Exercises – Alternate Short Periods of Activity and Rest
– Comfortable Postures
– Extension (Sloppy Push-Ups)

Not Recommended
• Complete Bed Rest
• Massage
• Chiropractic
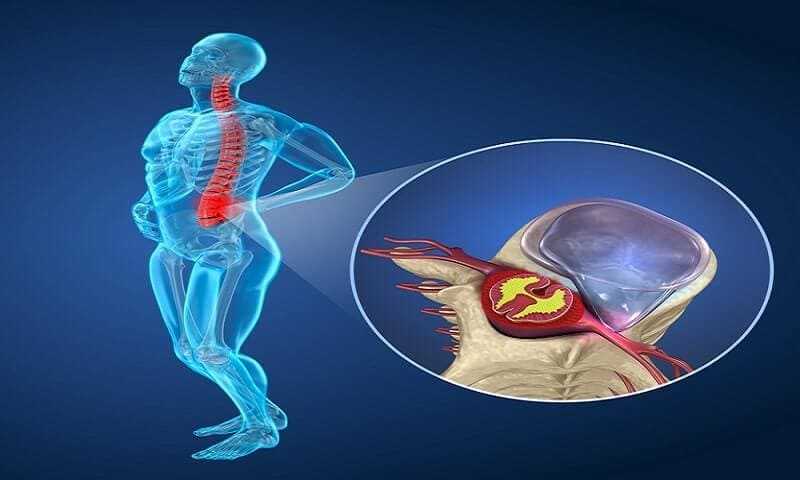
Treating Unresolved Sciatic Pain
The estimated lifetime incidence of sciatica in the general population is around 40%, while the incidence of disc surgery is only 1 % to 2%. Part of this difference relates to the fact that not all sciatica is due to a well-localized and identifiable disc herniation, but a significant factor is spontaneous resolution. The mechanism of non-surgical recovery involves resorption of the disc material, regression of the inflammation and swelling, along with recovery of the injured nerve.
Surgery: Identification of a specific, well-localized disc herniation in a young individual, where the pathology correlates with the clinical findings, may warrant early surgical intervention. Operating before 6 weeks is unusual, except in cases of cauda equina syndrome or progressive nerve loss with major muscle weakness, while evidence indicates a poor outcome once symptoms have been present for over 6 months. This may result from development of scarring around the nerve, chronic changes to the nerve itself, or persistent activation of central pain pathways.

Epidural Steroid Injection: In less clear-cut cases or where the patient is not keen to undergo surgery, consideration of epidural steroid injection should be made. There is sufficient research to support this procedure in specific instances with careful, X-ray guided technique. It can reduce pain significantly, allowing progression of activity and rehabilitation.

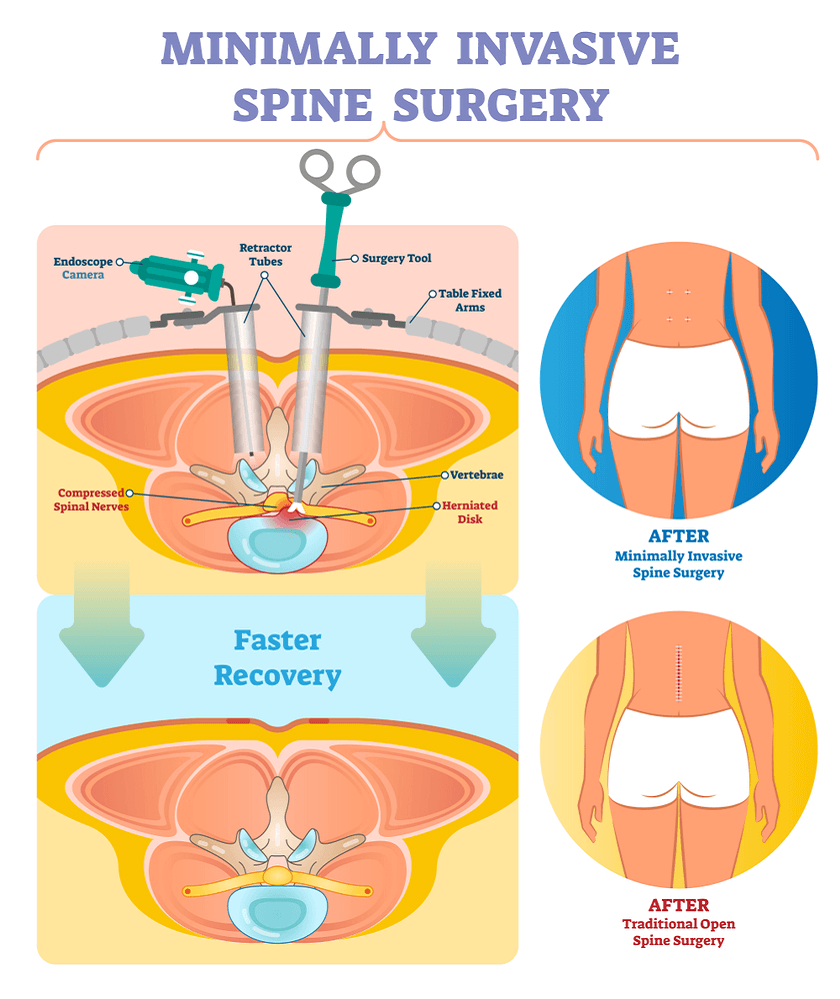
Minimally Invasive Procedures: Alternatives to surgical discectomy, the mainstay and accepted ‘gold standard’ of treatment, include minimally invasive procedures such as chemonucleolysis, percutaneous laser or suction discectomy, and arthroscopic discectomy.
What You Should Know About Minimally Invasive Spine Surgery ?
Recovery
The natural history of disc herniation varies according to a number of factors, including the size, type, and location of the herniation, the existence of other pathology such as arthritis, and the time-frame of development. For the uncomplicated posterolateral lumbar disc herniation without other spinal pathology, nearly 50% of individuals will show significant improvement in 2 weeks, and 70% in 6 weeks. (Other studies have shown 40% by one month, 50% by 2 months, and 70% by 3 months). Only between 10% and 20% have persistent radicular symptoms.
Sciatic Pain Facts
Only a small percentage of individuals with ‘sciatica’ end up needing surgery. However, sciatic pain that fails to resolve or improve considerably within the first 4 to 6 weeks is an indication for investigational imaging and more aggressive treatment.
Prevention
Activity and Exercise: As the pain from a herniated disc settles, activity can gradually be increased. Bending, twisting and lifting should be avoided in the short term but overall activity and exercise should progress. A back extension program should be continued and the strengthening component increased. Once the pain has settled completely, a full core-conditioning program can be started, advancing slowly with particular caution applied to flexion exercises, which should be delayed if they cause any recurrence of the original pain. Improved aerobic conditioning and weight loss may also aid in prevention of recurrence. Incorporation of Yoga or Tai Chi into a daily routine can be considered. Long-term ergonomic changes in posture, lifting technique, and other strenuous activity can help reduce the risk of recurrence.

Supplements: Although ongoing supplementation with essential fatty acids and vitamin B can have more general health benefits, they can be stopped about 3 weeks after the sciatic pain has completely resolved. Glucosamine and MSM can be taken long term and may provide some protective effect, although this has only been demonstrated in arthritis.