Ankylosing Spondylitis: Inflammatory Back Pain

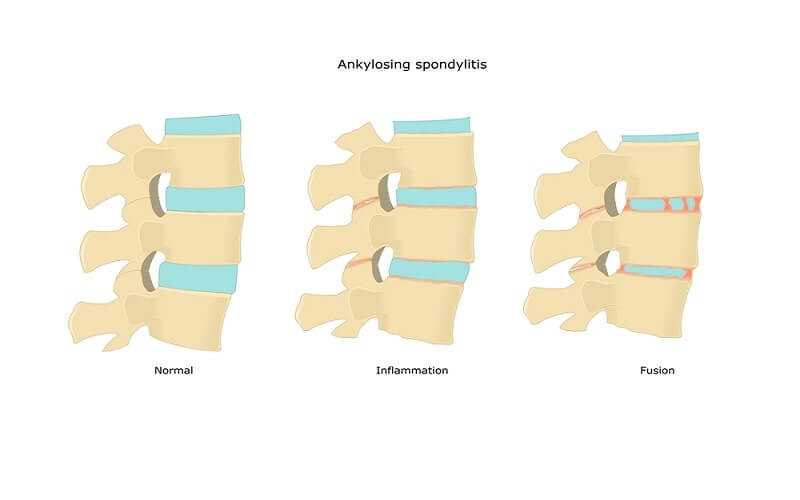
Ankylosing spondylitis is a form of inflammatory arthritis that affects the spine and sacroiliac joints. Spondylitis means inflammation involving joints of the spine and is derived from the Greek word for vertebra (spondylos) and inflammation (itis). As the inflammation subsides, healing takes place, with the bone growing out from both sides of the joint, eventually surrounding it completely. The joint is then unable to move and this stiffening is called ankylosis.

“Oh my aching back!” is the second most frequently heard medical complaint on earth, after the common cold, with 65 to 80 percent of the world’s population suffering back pain at some time during their lives. Ninety percent of back pain is caused by the overuse of muscles or a trauma; it goes away on its own without any treatment. That’s one reason why ankylosing spondylitis may go unrecognized for months or even years. The early back pain and morning stiffness of ankylosing spondylitis are often mistakenly treated as a form of back strain. Indeed, some people go through their lives with back complaints that are never correctly diagnosed as ankylosing spondylitis.
Nearly two million people in the U.S. have ankylosing spondylitis, a disease that’s been around at least three thousand years, with evidence of its presence having been observed in some Egyptian mummies. It generally strikes people in their late adolescence or early twenties, and men tend to be afflicted about twice as often as women. This form of inflammatory arthritis is included in a family of diseases called spondylarthropathies, which attack the spine. In addition to ankylosing spondylitis, these diseases include Reiter’s syndrome, some cases of psoriatic arthritis and arthritic inflammatory bowel diseases.
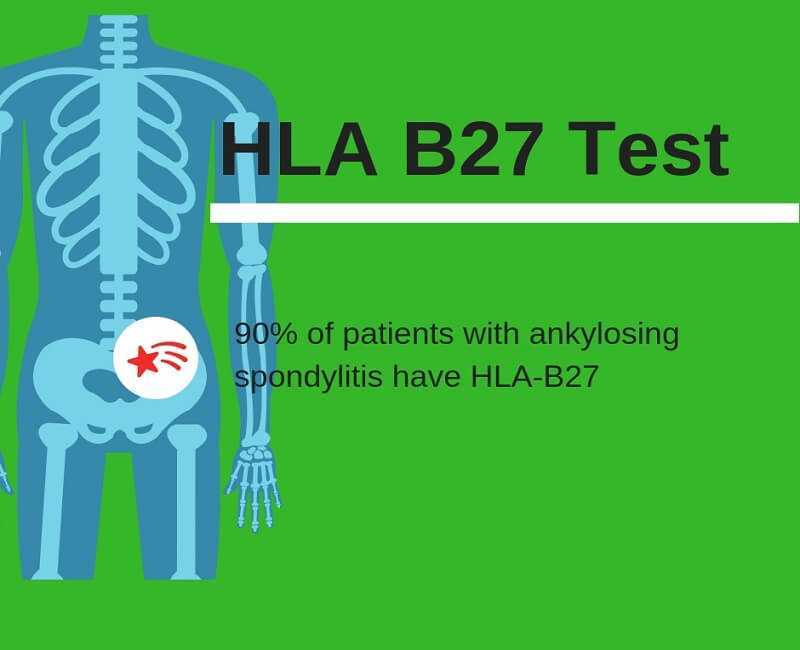
The cause of ankylosing spondylitis is still unknown, but all of the spondylarthropathies do share a common genetic marker, the white cell blood group that is numbered HLAB27. Ankylosing spondylitis is three hundred times more common in people who have the HLA-B27 gene than among those who do not. This means that virtually all people with ankylosing spondylitis will have HLA-B27. However, the reverse is not true. All people with the HLA-B27 marker will not have ankylosing spondylitis. Indeed, there are far more people with the blood group who will never get ankylosing spondylitis than there are people who do get it: it is estimated that more than 95 percent of those who are HLA-B27 positive never develop the disease. The HLA-B27 gene occurs in 7 to 10 percent of populations of European origin and appears much less frequently in African and Japanese populations. However, the gene can occur as high at 50 percent in North American Indian populations.

Since the gene runs in families, it is not unusual for more than one family member to have the disease. In fact, over one half of patients with ankylosing spondylitis have another family member who has the disease. The HLA-B27 gene does not cause ankylosing spondylitis, but people with the gene are more susceptible to getting the disease. It is believed that an intestinal infection from one or more unknown bacteria may trigger ankylosing spondylitis in susceptible people. Researchers are at work trying to identify which bacteria are involved. In some cases, the disease has occurred in those predisposed people after exposure to bowel or urinary tract infections.
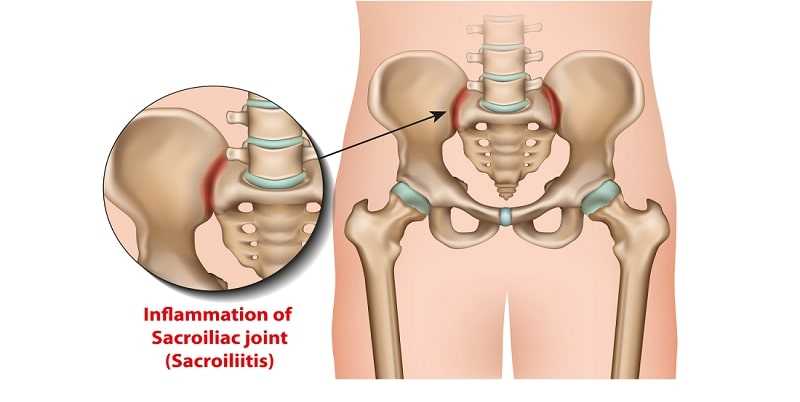
Symptoms of ankylosing spondylitis usually begin in late adolescence or early adulthood, at approximately twenty to twenty-five years of age. Often, the symptoms are ignored, attributed to growing pains or youthful exertion. Typically, ankylosing spondylitis originates in the sacroiliac joints, where the vertebrae of the spine meet the pelvis. The most common and early complaint is chronic lower back pain that starts gradually and persists for more than three months rather than coming in attacks. This back pain is dull in character and is felt primarily deep in the gluteal region and lower part of the back during the early stages. There is also stiffness in the back that is worse in the morning and then eases after mild physical activity or a hot shower. There may also be pain and stiffness after a prolonged period of sitting, for example, in a movie theater or on a long car ride.
These symptoms are in contrast to the symptoms of back pain that occur as the result of mechanical causes, which include: a sudden rather than gradual onset; pain that is localized across the lower back; usually no stiffness in the morning; the onset of symptoms occurring at any age, with a kind of back pain that usually is made worse by exercise but that can be relieved by prolonged bed rest.
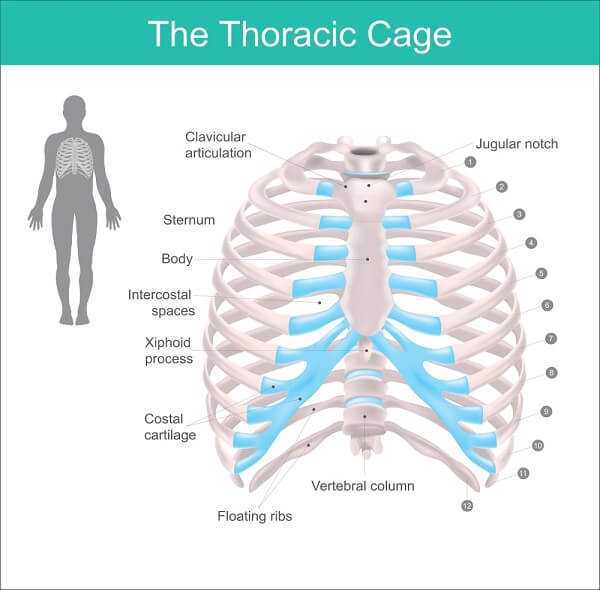
Ankylosing spondylitis produces an ache that is felt in the buttocks and, sometimes, down the backs of the thighs and in the lower part of the back. One side is commonly more painful than the other and arises from the sacroiliac joints. The disease tends to progress from the lower back up to the vertebrae in the neck. Pain is not always confined to the back. Some patients have chest pain, which worsens on deep breathing and is felt around the ribs. This chest pain does not come from the heart but from the joints between the ribs and the backbone. For many, it feels difficult to move the ribs fully when breathing deeply, although the lungs can continue to work because the diaphragm is not affected. In severely affected patients, when the rib cage does not move well, pneumonia can develop.
Sometimes, either at the beginning or later on, ankylosing spondylitis may affect joints other than in the spine, including the shoulders, hips, knees, ankles and feet. Also, certain tender places may develop in bones that are not part of the spine. One of these is the heel bone, which makes it uncomfortable to stand on a hard floor, and another is the bone of the seat, making hard chairs unpleasant. In approximately one out of seven patients, attacks of inflammation of the eye will occur.

There is no diagnostic test that can be given at the onset of back pain to confirm the presence of ankylosing spondylitis. A description of the patient’s symptoms, which differ from those of mechanical back pain, should alert the doctor to consider that a patient may be developing ankylosing spondylitis. Additionally, identification of the HLA-B27 gene factor would provide additional positive data for consideration. In addition to taking a history of symptoms, the doctor will examine the patient, looking for muscle spasm and noting posture and mobility in the back, along with reviewing other parts of the body for evidence of the disease.
A diagnosis of ankylosing spondylitis can be confirmed from an X ray taken of the sacroiliac joints, if these reveal changes in tissues that are caused by inflammation. However, these tissue changes don’t always appear on X rays during the early stages of the disease. The doctor will also probably test for anemia and perform a test called the erythrocyte sedimentation rate (ESR), which tells how active the disease is.

Since early treatment is critical to reduce uncontrolled inflammation and pain and to prevent long-term deformities, an experienced physician will often diagnose the disease and begin treatment even before the x-ray findings are conclusive, relying on symptoms, the presence of the HLA-B27 gene and the physical examination.

No two cases of ankylosing spondylitis are exactly the same, the disease takes a different course in different people, and the symptoms may come and go over long periods. But eventually ankylosing spondylitis becomes less severe. However, the lumbar spine usually becomes stiff and the upper part of the back and the neck can stiffen as well. The worst disability resulting from ankylosing spondylitis is fixation of the back in a bent or stooped position. This used to be quite common in ankylosing spondylitis patients but is now prevented by early diagnosis and treatment.
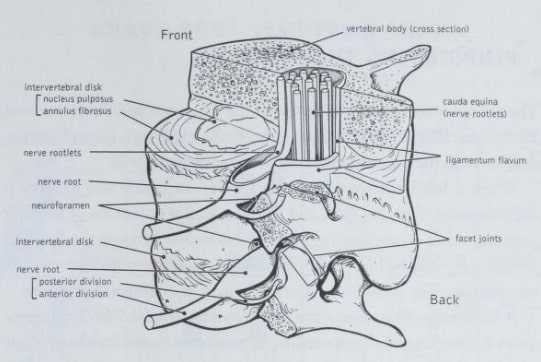
Over time, the inflammation at the ends of the ligaments results in stiffness, and movement becomes painful. After a period of stiffness and pain, a bony bridge grows between the parts, and the area becomes totally rigid. This fusion stops motion but has the beneficial effect of eliminating pain since pain is experienced only in areas that are still able to move.
In contrast to rheumatoid arthritis, which can cause destruction of the bones around a joint, ankylosing spondylitis fuses the intact bones together. This bony fusion can be extensive in the most severely affected patients and can lead to the creation of a single giant bone that includes the pelvis, the spine, the skull and the ribs, leaving the central part of the body without any motion at all. People who do develop a stiff or “ankylosed” spine will nevertheless remain functional if this fusion occurs in an upright position. Probably the most common significant limitation is a fusion of the neck in a flexed position, which limits the person’s ability to raise the head.
Traditional Treatments
Since there is no cure for ankylosing spondylitis, the doctor will aim to relieve the symptoms, improve spinal mobility where it may have been lost and help a patient pursue a normal occupational and social life. Although the disease tends to become less active in later years, the treatment really continues forever. In addition to taking medication for the relief of pain and inflammation, a patient will need to incorporate physical therapy, exercise, diet, rest and posture control into a daily routine. This combination of antiinflammatory medication and a sustained program of exercise can slow down the progression of the disease and enable the patient to maintain activity.
Drug treatment As a way of relieving any pain and inflammation, helping to get a good night’s sleep and gaining sufficient freedom from pain to take part in an exercise program (another critical element of successful therapy), drug treatment can be an important element in any treatment plan for patients with ankylosing spondylitis. Nonsteroidal anti-inflanmiatory medications (NSAIDs) generally provide the most effective results. Indomethacin is most commonly prescribed, and is available in a suppository to counter early morning stiffness. Because it has serious side effects, phenylbutazone is used only when other NSAIDs have failed.

Many patients find that they need continuous treatment on a small maintenance dose of their drug. Some of the newer tablets are manufactured to remain effective throughout the night and into the first part of the day.
Good posture An important element of an ongoing treatment program for ankylosing spondylitis is the maintenance of good posture, in order to prevent progressive stooping from flexion of the spine. Although it is rare for the spine to stiffen completely, a conscious effort towards maintaining good posture will ensure that if it does happen, at least it stiffens in an erect rather than a bent position. You must develop the habit of being aware of your posture and being sure to correct it constantly, not only during exercise periods but throughout the day, while standing, sitting and walking.

At home, to maintain good posture while sitting, select a chair that has a firm seat, straight back and armrests. There should be firm rather than soft padding on the seat and back. The seat of the chair should not be too long from front to back because this will make it difficult to place your lower spine into the base of the back of the chair. Don’t sit for long in low, soft chairs, as this will result in bad posture and increased pain.
At the office, pay special attention to the position of your back so that you do not have to stoop. Make sure that your seat is at the proper height and do not sit in one position for too long without moving your back. A job that allows a variety of movements—sitting, standing and walking—is ideal. Most unsuitable would be a job where you would have to stoop or crouch over a table or a computer console for hours at a time. If you do have a job that keeps you in one place for long periods of time, make sure you get up at least every hour and stretch and walk around. It would be ideal to be able to lie flat for fifteen minutes at midday.
If you have to make a long journey in a car, it’s very important to stop for five minutes every hour or so and get out of the car for a stretch. This is not only beneficial for maintenance of your posture, it’s also a safety factor since pain and stiffness can distract your attention from driving. Patients who have stiffness of the neck and other parts of their spine have difficulty backing into parking spaces because they can’t turn easily to look behind them. Special mirrors are available to fit onto your car that can help. Headrests for the front seats are also advised so that sudden deceleration injuries to the neck can be avoided. A stiff neck is more easily hurt than a normal neck.
When lying in bed, it is important to be flat on your back; also practice lying face down some of the time. This prone lying, as it is called, should be done for twenty minutes in the morning and twenty minutes before going to bed at night. At first, you might not be able to tolerate more than five minutes of prone lying at a time or perhaps you may need a pillow under your chest. With practice, as the spine relaxes, it becomes easier. Making a habit of this will help to prevent your back and hips from becoming bent.
The bed you sleep on should be firm, without a soft or sagging mattress. A sheet of plywood or chipboard two feet by five feet by one half inch is ideal to place between the mattress and the bed frame. Not only is a firm bed more comfortable to lie on than one that is yielding, but it will help prevent any tendency for spinal curvature to develop later on.

Physical therapy In order to maintain mobility of the joints affected by ankylosing spondylitis, regular physical therapy is vital. Ideally, a physical therapist, in consultation with your doctor, will design ein exercise routine tailored to your individual requirements. Once you have learned the exercises, try to do at least some of the routine, if not all of it, every day. Exercise helps to make you conscious of your posture, especially the position of your back, and also encourages free movement of certain joints, especially the shoulders and hips. It is important to keep muscles strong, because reduced movement, even for a short time, allows them to become weaker, and it takes a long time to build them up again. Here are some suggested exercises:
1. Standing with your heels and seat against a wall and keeping your chin in, push your head back towards the wall and keep it back for the count of five, then relax. Repeat ten times.
2. Sit on a firm chair, put your right hand across your chest and hold the side of the chair. Stretch your left arm out in front of you and then twist to the left, taking the arm horizontally as far behind you as possible, turning your head to look over the left shoulder. Hold this position, then push and turn a little further, hold that position and then return to facing forward. Repeat three times with each arm.
3. Sit with your shoulders relaxed and chin drawn in, looking straight ahead. Bend your head sideways to bring your right ear toward your right shoulder, hold it here, make sure your shoulder muscles are still relaxed and bend a bit further, then return to straight. As you do the side bending, the profile of your nose should remain in the same place, to make sure you don’t turn your head. Repeat, bending to each side twice.
Now tip your head back, looking up the wall and along the ceiling and bring it back to straight. Repeat.
Change to tipping your head forward as far as possible to get your chin touching your neck, and return to straight with chin pulled in. Repeat once.
4. Lie on your back with knees bent up, lift up your hips so your seat is off the floor and there is a straight line from shoulder to knees. Hold for the count of five, and lower. Repeat five times.
5. Lie on your stomach, head turned to one side, hands by your sides. If necessary, you may put a pillow under your chest, but not at your waist, in order to get comfortable. Raise one leg off the ground, keeping your knee straight. Repeat five times with each leg, making sure your thigh comes off the ground. Raise your head and shoulders off the ground as high as you can ten times.
6. Kneeling on the floor on all fours, lift and stretch the opposite arm and leg out parallel with the floor and hold for the count of ten. Lower and then repeat with other arm and leg. Repeat five times each side.
7. Lie on your back with your legs straight. Put your hands on your ribs at the sides of chest. Breathe in deeply through your nose and out through your mouth, pushing your ribs out against your hands as you breathe in. Repeat ten times. Remember, it is as important to breathe out fully as it is to breathe in deeply.
Put your hands on the upper part of the front of your chest. Breathe in deeply through your nose and then breathe out as far as you can through your mouth. Push your ribs up against your hands as you breathe in. Repeat ten times.
Sports should be an important element of your physical therapy program. The ideal sport for an ankylosing spondylitis patient is swimming, since it uses all the muscles and joints without janing them. Contact sports are not ideal, because the joints can get injured. Golf has drawbacks, because players may spend long periods putting, during which the spine is in continued flexion. Basketball and volleyball are excellent, as they combine movement with stretching and jumping. Another excellent activity is cycling, because it helps to keep the joints active and strengthens the muscles in the legs. It also provides good breathing exercise and helps the rib cage continue to expand. Be sure that the handlebars of the bicycle are adjusted so the rider is sitting tall, not hunched over.
Surgical procedures Surgery is occcisionally used in correcting late spinal deformities in the back or neck when they are so severe that the patient cannot look forward and has difficulty crossing the road. This operative treatment may not be possible in some instances, though, because of the difficulty of safely giving anesthesia in a patient with severe ankylosing spondylitis. Total hip replacement is a more frequent surgical treatment, for a patient who has become disabled by deterioration of the joint.

Adaptive aids and devices Patients who face severe lifestyle restrictions in the wake of irreversible deformities can facilitate the performance of many activities through the use of specially designed adaptive aids and devices. For example, when the neck and back are flexed so far forward that walking and reading are difficult, prism glasses can improve the field of vision. Ambulation aids, such as canes, can also help to maintain activity and prevent falls. Special rearview mirrors can be installed on automobiles to help increase visibility for patients who drive. A contoured cervical pillow and lumbar-roll cushion can help patients maintain good posture while sleeping.
Counseling In a long-range treatment program for a person with ankylosing spondylitis, counselors, including specialists in physical therapy and occupational therapy, can help fashion the kinds of exercise programs and adaptive adjustments that will make life more manageable. Also, by joining ankylosing spondyhtis patients’ groups, sufferers can gain emotional support, accurate information and greater understanding of the disease.
Diet A treatment program for ankylosing spondylitis should include an emphasis on good nutrition and weight control. The latter is important for maintaining overall good health and energy as well as for protecting the joints from the strain of added weight. Recommended daily are two helpings of protein food, fruits, vegetables and other foods that are the source of vitamins and calcium.

Heat The pain and stiffness of ankylosing spondylitis in the spine and neck can be alleviated by the application of heat. A hot bath before retiring or a hot water bottle or electric blanket in bed are usually adequate.
Alternative Treatments
The traditional approach to treating ankylosing spondylitis is an ongoing, multifaceted treatment program, combining medication, physical therapy, exercise, diet and posture control. Since a patient must plan on continuing treatment over a lifelong term, the incorporation of alternative methods within the program can help to add variety and interest.
Certain mainstays of alternative healing, however, should be avoided. For example, spinal manipulation should not be undertaken, as there is a real danger of severe harm occurring to the spinal column.
Most beneficial to ankylosing spondylitis patients are those therapies that emphasize relaxation of tensions, relief from pain and maintenance of a positive outlook.
Alexander Technique A philosophy emphasizing the need to releam the natural body posture that one was bom with and that has been undone over the years through stress, improper breathing and general abuse of posture is the Alexander Technique. No manipulation of the spine is involved, with the emphasis being on posture and breathing, so the technique should be safe for ankylosing spondylitis patients. Before consulting with an Alexander teacher, however, you should talk with your doctor and see if there are any restrictions you should know about.

Relaxation techniques There are daily tensions that tighten up muscles and even the ability to breathe deeply. which can exacerbate efforts to maintsdn good posture. Relaxation techniques can loosen muscles and smooth breathing. Try techniques such as meditation, music, etc., until you find one that works best for you.
Combined Treatments
When faced with maintaining a treatment program for a chronic, incurable disease like ankylosing spondylitis over a period of perhaps thirty or forty years, it’s very important to keep your daily routine fresh and appealing, especially the elements of your daily exercise program, because the persistence of your efforts is directly related to long-term success in lessening deformities. Therefore, you must see your doctor regularly to maintain an accurate gauge of how well things are working and what changes ought to be made.
Also, it’s very important to keep up-to-date with the latest findings in research, treatment options and the experiences of other patients. Just applying on a daily basis all of the traditional therapies that are advised for an ankylosing spondylitis patient will leave little time in the day to add alternative treatments. However, when a highly praised technique does seem worth trying, discuss it with your doctor to see how you might best try it out.