Chronic Pain From Shingles
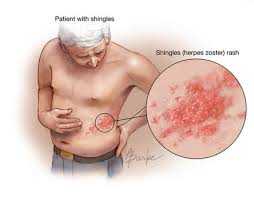
Shingles is the common name for a Herpes Zoster infection of the skin (see image).
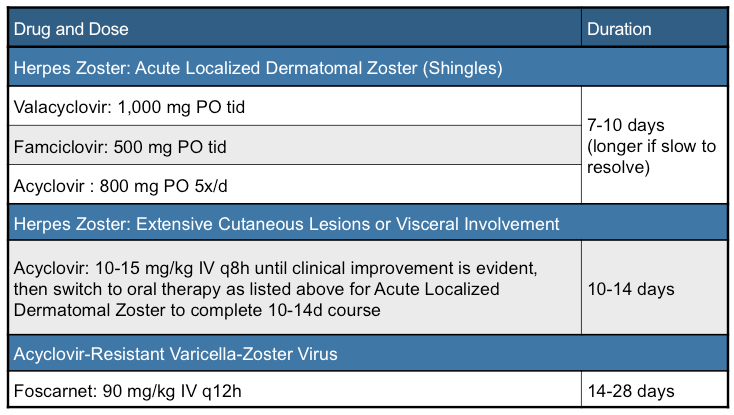
There is a 18% likelihood that all adults who develop this infection will develop chronic pain from it. Less than 10% of adults under the age of 60 years old develop the syndrome.
If you are over 60 years of age and develop shingles you have a 40% likelihood of developing the syndrome. The pain is called a Post-Herpetic Neuralgia. That pain can be very disquieting and difficult to treat.
What Are “SHINGLES”?
Before 1995, there were over 11,000 hospitalizations and 100 deaths due to Chickenpox per year in the U.S.. The Chickenpox vaccine was released for use in 1995 and has substantially reduced the incidence of clinical Chickenpox.
Chickenpox is usually contracted as a child and results in a mild blistering rash. It runs its course in 5 to 10 days. The child is very contagious until the last blister is scabbed over. Disfigurement is uncommon (unlike smallpox). The primary infection resolves on its own.
The virus then goes into a dormant phase where it hibernates for years in the brain and spinal cord. Under certain conditions the virus is “reactivated,” migrates from its locations of hibernation, and recurs not as a systemic blistering rash but as an intense local, pustular rash.
The rash is usually located on the side of the face, chest, abdomen, arm, or leg. It is extremely painful.
Prior to development of the pustular rash the symptoms can be very non-specific. A normal skin appearance with burning or tingling, sensitivity to touch, itching, fever, headache, fatigue, and sensitivity to light are all symptoms that may precede the rash.
The rash follows and causes significant irritation and damage of the nerves involved. The skin can also be very scarred from the pustular eruption once it heals.
Most people who develop shingles have a lowered immunity for some reason. Psychological stress, over 60 years of age, certain cancers, HIV, and medications that lower the immunity can place a person at risk for developing Shingles.
Who Gets Chronic Pain After a Case Of “SHINGLES”?
Not everyone who develops the painful rash develops chronic pain. As said previously, the over 60 year old individual who develops the skin infection of Herpes Zoster (Varicella is in the Herpes family) has a 40% chance of developing the prolonged pain syndrome. This is especially true if left untreated.
Caucasians are 3 times more likely to develop the neuralgia as African Americans. Older, debilitated, or immune compromised people have a much higher likelihood of developing the syndrome also.
How Is Post-Herpetic Neuralgia Diagnosed?
After the pustular rash has healed the pain usually remits. If the burning pain continues for 1 – 3 months, after the rash is healed, the person is said to have a Post-Herpetic Neuralgia. The intensity of the pain can can vary.
There is no particular diagnostic study that is used for this syndrome. It is clinically diagnosed after having had an episode of Shingles.
Curiously, studies have shown that patients with a robust pustular skin reaction have a 56% likelihood of having an abnormal MRI with lesions in the brain stem and cervical spinal cord.Patients with these findings have a much higher possibility of developing the neuralgia.
None of the patients with Shingles who had normal MRIs developed neuralgia.
Can Herpes Zoster Be Treated?
The best way to “treat” Post Herpetic Neuralgia is to avoid developing the pustular skin infection. The Chickenpox Vaccine (Zostavax) has been effective in reducing the incidence of Shingles in people over 60 years of age and is recommended as a routine vaccination.
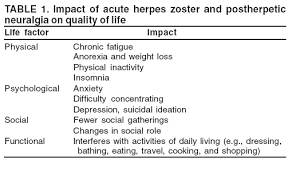
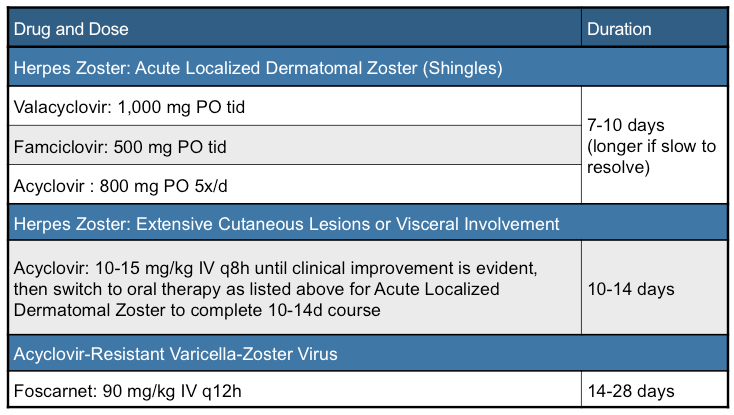
Once the rash has developed, an anti-viral antibiotic specific for Herpes Zoster will improve the healing of the rash if given at the onset of the pustular eruption (see the above table). These prescriptions can be obtained from a Primary Care Practitioner.
If the rash is allowed to run its course without antibiotic treatment, the painful syndrome is more likely to occur. Treatment of the pain becomes the primary focus.
TREATMENT OF POST-HERPETIC NEURALGIA
1) Agents Applied To The Skin:
- Lidoderm skin patch which is a local anesthetic agent applied directly to the skin.
- Specially made preparations by a boutique pharmacy that mix 3 or more medications together to be directly applied to the skin.
2) Agents Taken By Mouth:
- Anti-inflammatories (click here to see my post on this topic)
- Acetaminophen
- Opiate pain medications
- (click here to see my post on this topic)
- Anti-depressants (such as Cymbalta…click here to see my post on this topic)
- Anti-convulsants
- Homeopathic supplements (Magnesium…click here to see my post on this topic)
3) Acupuncture (click here to see my post on this topic)
4) Relaxation Techniques
5) Hot/Cold Packs
6) Trans-cutaneous Electrical Nerve Stimulation (TENS…click here to see my post on this topic)
7) Spinal Cord Stimulator(Magnesium…click here to see my post on this topic)
Summary Remarks
We have reviewed the Shingles skin infection, risk factors for developing the chronic pain of Post-
Herpetic Neuralgia, and treatment modalities. In the U.S. the chronic pain syndrome can be avoided by vaccination or early treatment with antibiotics for the pustular skin eruption.
Effective treatment for the pain after the neuralgia develops is more challenging. Most people will respond to multiple overlapping treatments. Today there is great hope for pain relief if a person develops Post-Herpetic Neuralgia.
To your health!