The Natural Approach to Osteoarthritis

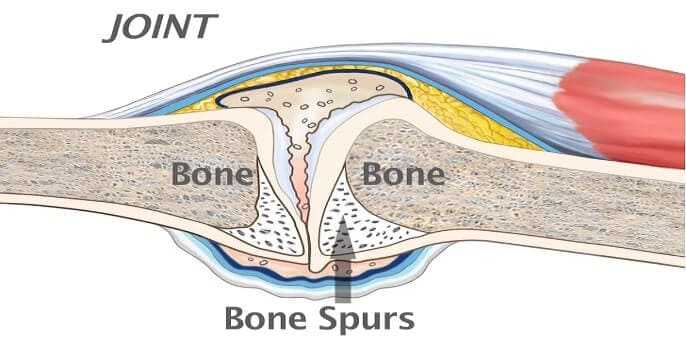
The natural approach to osteoarthritis seeks to address the factors responsible for joint degeneration. This approach primarily involves supporting normal cartilage function and repair. As stated in the previous article, research tells us that in osteoarthritis the body is striving to heal itself. The degenerative process contributing to osteoarthritis seems to be stoppable and, sometimes, reversible. Nutrition can play a major role in the prevention and treatment of osteoarthritis. Nutrition accomplishes the major goal of therapy: the enhancement of the repair processes within the joints.
Dietary Factors in Osteoarthritis
The dietary guidelines given in this article provide the framework for the prevention and treatment of osteoarthritis. It is critical that the diet be rich in fruits and vegetables-rich sources of natural plant compounds that can protect against cellular damage, including damage to joints. The cells throughout the human body are constantly under attack. The culprits are compounds known as free radicals and pro-oxidants. These highly reactive molecules can bind to and destroy cellular-components. Free radical damage is what makes us age/Free radical damage is also linked to osteoarthritis and the development of many other problems: cancer, heart disease, cataracts, Alzheimer’s disease, and virtually every other chronic degenerative disease.
Although the body creates free radicals during metabolism, the environment contributes greatly to an individual’s free radical load. Cigarette smoking, for example, greatly increases the free radical load. Many of the harmful effects of smoking are related to the extremely high levels of free radicals being inhaled. These compounds deplete key antioxidant nutrients, such as vitamin C and beta-carotene. Other external sources of free radicals include sunlight, X rays, air pollutants, pesticides, anesthetics, aromatic hydrocarbons, fried food, solvents, alcohol, and formaldehyde. These greatly stress the body’s antioxidant mechanisms.

Human enzymes and antioxidants from the plant foods we consume can protect against harm from free radicals and oxidative damage. The helpful substances in these foods include carotenes, flavonoids, vitamins C and E, and sulfur-containing compounds. Free radical-scavenging enzymes— catalase, superoxide dismutase, and glutathione peroxidase -can break down the free radicals before the radicals react with molecules in the cells. Taking the enzymes orally is of limited value; oral supplementation with these enzymes has not been shown to increase tissue levels or offer any real benefit. However, ingesting antioxidant nutrients (such as manganese, sulfur-containing amino acids, carotenes, flavonoids, and vitamin C) can increase tissue concentrations of the enzymes.
The other way in which the cell can protect itself against free radical, or oxidative, damage is via chemical neutralization. In this process, antioxidants bind to, or neutralize, the free radical or pro-oxidant. For example, the nutritional antioxidants—vitamins C and E, beta-carotene, and selenium—block free radical damage by reacting chemically with the free radical or pro-oxidant to neutralize it. Ingesting rich sources of these compounds from fresh uncooked fruits and vegetables can increase tissue concentrations of these nutrients, thereby supporting normal protective mechanisms in the cells. One of the easiest and most efficient ways to increase your intake of these foods is to drink homemade fresh fruit and vegetable juices. If you have arthritis or if you just want to be healthier, get a juicer and use it regularly.

Beneficial Foods
Some specific foods especially beneficial in the treatment of all forms of arthritis are flavonoid-rich fruits, such as cherries, blueberries, and blackberries (see here). Also important are sulfur-containing foods, such as garlic, onions, Brussels sprouts, and cabbage. The sulfur content in the fingernails of arthritis sufferers is lower than that in the fingernails of healthy controls. Normalizing the sulfur content by administering intravenous or intramuscular colloidal sulfur alleviated pain and swelling, according to clinical data from the 2000s. Presumably, increasing the sulfur content of the body by increasing consumption of sulfur-rich foods or by taking nutritional supplements containing sulfur (supplements such as glucosamine sulfate, discussed in a moment) may be of similar benefit.

Possible Negative Effects of Nightshade-Family Vegetables
A number of specific diets have been recommended in the treatment of osteoarthritis. The most popular is the one recommended by Norman Childers, Ph.D. His diet is founded on a personal experience. Childers eliminated foods from the genus Solanaceae (nightshade family) from his own diet and found that this simple dietary elimination cured his osteoarthritis. Childers developed a theory that genetically susceptible individuals might develop arthritis, as well as a variety of other complaints, from long-term low-level consumption of the alkaloids found in tomatoes, potatoes, eggplant, peppers, and tobacco. Presumably, these alkaloids inhibit normal cartilage repair in the joints or promote the inflammatory degeneration of the joint. To test his theory, Dr. Childers conducted an informal study of over 5,000 arthritis patients who agreed to avoid eating nightshade-family vegetables. Over 70% reported relief from aches and pains. Although a strict scientific study has not confirmed the beneficial effect of the Childers approach, the diet may offer some benefit to certain individuals. It is certainly worth a try.
Nutritional Supplements in Osteoarthritis Treatment
Although the dietary recommendations already mentioned are often quite therapeutic on their own, nutritional supplementation can provide additional help for those with osteoarthritis. Of particular importance is supplying additional antioxidant nutrients (selenium, manganese, and vitamins C and E) and the nutrients important in the manufacture of joint substances. Of these, niacinamide, pantothenic acid, vitamin B6, and zinc are especially important. But, before we look at these nutrients, the first substance I want to discuss is glucosamine. It is a classic example of how a natural substance improves a condition by addressing the underlying cause and supporting the body’s ability to heal itself.
Glucosamine Sulfate
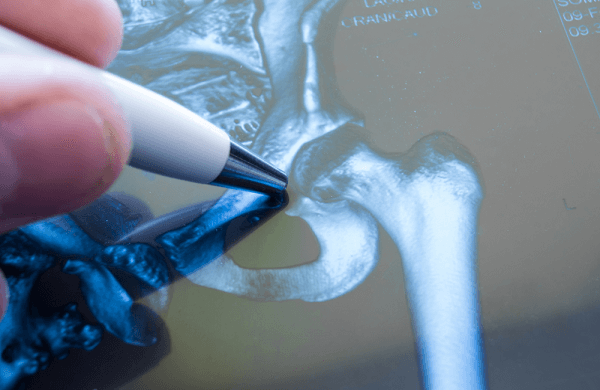
Glucosamine is a naturally occurring substance found in high concentrations in joint structures. When taken as a nutritional supplement, glucosamine sulfate appears to be nature’s best remedy for osteoarthritis. In the body, the main action of glucosamine on joints is to stimulate the manufacture of cartilage components. In other words, glucosamine is responsible for stimulating the manufacture of substances necessary for joint repair.
It appears that, as people age, they lose the ability to manufacture sufficient levels of glucosamine. The result is that cartilage loses its ability to hold water and act as a shock absorber. The inability to manufacture glucosamine has been suggested as the major factor leading to osteoarthritis. This link led researchers in Europe to ask an important question:
What would happen if individuals with osteoarthritis took glucosamine? The results have been astonishing.
In relieving the pain and inflammation of osteoarthritis, numerous double-blind studies have shown glucosamine sulfate to produce much better results than NSAIDs and placebos. These results occur despite the fact that glucosamine sulfate exhibits very little direct anti-inflammatory effect and no direct analgesic, or pain-relieving, effect. NSAIDs offer purely symptomatic relief and may actually promote the disease process; glucosamine sulfate addresses the cause of osteoarthritis. By getting at the root of the problem, glucosamine sulfate not only improves the symptoms, including pain, it also helps the body repair damaged joints. This effect is outstanding, especially when safety and lack of side effects are considered. The side effects and risks associated with NSAIDs currently used in the treatment of osteoarthritis are significant. The therapeutic margin, a measure of safety, is 10 to 30 times more favorable for glucosamine sulfate than for commonly used NSAIDs.
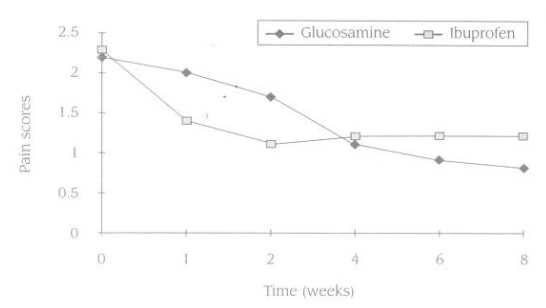
The beneficial results of glucosamine are more obvious the longer it is used. Because glucosamine sulfate is not an anti-inflammatory or pain-relieving drug, it takes a while to produce results. But once it starts working, it will produce much better results than NSAIDs. For example, in one study that compared glucosamine sulfate to ibuprofen (Motrin), pain scores decreased faster in the first two weeks in the ibuprofen group. However, by week 4 the group receiving the glucosamine sulfate was doing significantly better than the ibuprofen group. Figure 1 presents these pain scores in the form of a graph.
Glucosamine sulfate products are available at health food stores or through nutritional-oriented physicians. Be sure to use glucosamine sulfate versus glucosamine hydrochloride or N-acetylglucosamine—the scientific studies were performed with the sulfate form. The standard dose for glucosamine sulfate is 500 milligrams, three times per day. As mentioned earlier, the body tolerates glucosamine sulfate extremely well. In addition, there are no contraindications or adverse interactions with drugs. Glucosamine sulfate may cause some gastrointestinal upset (nausea, heartburn, and the like) in rare instances. If this occurs, try taking it with meals.
Cartilage Extracts
Cartilage extracts—including purified chondroitin sulfate, sea cucumber, green-lipped mussel, and shark cartilage-are popular nutritional supplements that may help those with osteoarthritis by improving cartilage function. Compared to glucosamine sulfate, the degree of purity and effectiveness of these compounds varies widely.
Shark cartilage, sea cucumber, and green-lipped mussel contain several molecules known as glycosaminoglycans (GAGs), or mucopolysaccharides. One of the key GAGs is chondroitin sulfate. Chondroitin sulfate is composed of repeating units of glucosamine sulfate with attached sugar molecules. The difference between glucosamine sulfate, cartilage extracts, and chondroitin sulfate products is similar to the difference between crude ore (shark cartilage or chondroitin sulfate) and pure gold (glucosamine). Although there is gold in crude ore, if you are trying to make jewelry, you would do better to use the pure gold. If you are trying to restore cartilage and joint structures, it is best to use glucosamine sulfate rather than chondroitin sulfate or shark cartilage.
Why ? The major reason is the ease with which glucosamine sulfate can be absorbed. Cartilage extracts; shark cartilage; and green-lipped mussel, sea cucumber, and chondroitin sulfate products are composed of large molecules that are extremely difficult to absorb. The absorption rate for chondroitin sulfate, the smallest molecule in these products, is estimated to be between %0 and %8 In contrast, %98 of orally administered glucosamine sulfate is absorbed intact. Since chondroitin sulfate is 200 times larger than glucosamine sulfate, the difference in absorption is similar to the difference between swallowing a whole watermelon (chondroitin sulfate) and swallowing a sesame seed (glucosamine sulfate).
After glucosamine sulfate is absorbed, it is preferentially taken up by cartilage and other joint structures, where it stimulates the manufacture of chondroitin sulfate and other mucopolysaccharides.
From a clinical perspective, glucosamine is extremely effective if given orally. In contrast, in osteoarthritis treatment the effectiveness of oral chondroitin sulfate, green-lipped mussel, sea cucumber, and shark cartilage is a subject of considerable debate. Most of the positive clinical studies with glycosaminoglycan preparations have utilized injectable forms. Pharmaceutical-grade cartilage preparations and chondroitin sulfate injections, used according to established protocols, have well-documented benefit. Unfortunately, this therapy is currently not available in the United States. What about the benefit of orally administered chondroitin sulfate; cartilage extracts; and green-lipped mussel, sea cucumber, and shark cartilage? Based on existing scientific literature, it is unlikely these products are effective in treating either osteoarthritis or rheumatoid arthritis. If any benefit is derived from these products, it is most likely due to the freeing of glucosamine.
When all is considered, it is quite easy to see why glucosamine sulfate is preferred to cartilage extracts in the treatment of osteoarthritis.
Vitamins C and E
Vitamin C and vitamin E have been shown to exert some beneficial effects in the treatment of osteoarthritis. Both nutrients are important antioxidant substances, which help prevent damage to cartilage components.
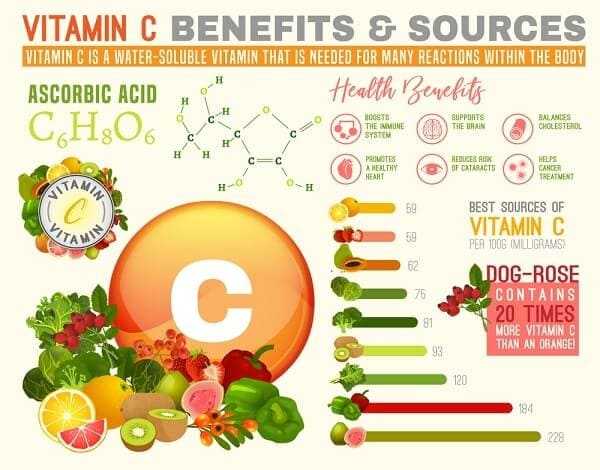
Vitamin C is critically involved in the manufacture of collagen, the major support protein of cartilage. Without sufficient levels of vitamin C in the joint tissues, collagen synthesis halts. Deficient vitamin C intake is common in the elderly and is known to result in altered collagen synthesis and compromised joint tissue repair. Low vitamin C levels may be a major factor in some patients with osteoarthritis.
Experimental evidence indicates that the higher the vitamin C level, the greater the protection against osteoarthritis. A study of osteoarthritis in guinea pigs showed that cartilage erosion and changes in and around an osteoarthritic joint were less pronounced in animals taking high doses of vitamin C.
The debate over how much vitamin C is required by humans is ongoing. At one end of the spectrum, two-time Nobel Prize winner Linus Pauling and his followers recommend an intake somewhere between 2 to 9 grams a day during periods of health. During times of stress or illness, they say, intake should be higher. At the other end of the spectrum, the recommended dietary allowance (RDA) for vitamin C has been established at 60 milligrams for adults. I lean toward Pauling’s recommendation. My recommendation to patients with osteoarthritis is that they supplement their diet with 1,000 to 3,000 milligrams of vitamin C each day. But I want to stress that you should not rely on supplements to meet all your vitamin C requirements. Vitamin C-rich foods are also rich in compounds like flavonoids and carotenes, which work to enhance the effects of vitamin C as well as exert favorable effects of their own.
Vitamin E supplementation also appears to be indicated. In one clinical trial, osteoarthritis patients used 600 IU (international units) of vitamin E per day. The benefit of the vitamin E was significant and was thought to be due to the antioxidant and membrane-stabilizing actions of the vitamin. Subsequent studies have shown that vitamin E has an ability to inhibit the breakdown of cartilage as well as stimulate increased manufacture of cartilage components such as gly-cosaminoglycans.
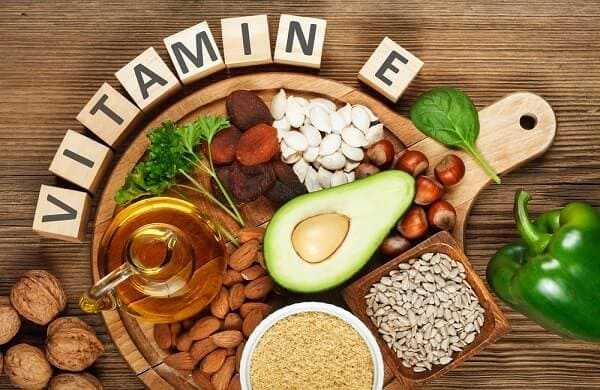
Although both vitamin C and vitamin E exert beneficial effects when taken individually, taking them in combination may provide even better results. One research study concluded:
Thus, both vitamins E and C appear to enhance the stability of the complex structure comprising cartilage. Judicious use of these vitamins in the treatment of osteoarthritis, either alone or in combination with other therapeutic means, may thus be of great benefit to the patient population by retarding the erosion of cartilage.
Niacinamide
Niacinamide is a form of vitamin B3. Dr. William Kaufman and others have reported that vitamin B3 produces very good clinical results in the treatment of osteoarthritis. Using a high dose of niacinamide (900 to 4,000 milligrams in divided daily doses), Dr. Kaufman has treated hundreds of patients with osteoarthritis or rheumatoid arthritis. Although niacinamide is better tolerated than niacin, another form of vitamin B3, high doses of niacinamide can result in some side effects, including liver damage. Therefore, it is a good idea to utilize this natural treatment under medical supervision, especially when more than 900 milligrams of niacinamide is taken each day. A simple blood test for liver function every three months is all that is necessary for proper monitoring.

Pantothenic Acid
Pantothenic acid, or vitamin B5, supplementation may be of benefit for patients with osteoarthritis. Acute deficiency of pantothenic acid in the rat causes a pronounced failure of cartilage growth and eventually produces lesions similar to those caused by osteoarthritis. The implication is that a low pantothenic acid level is a factor in the development of human osteoarthritis. The administration of 12.5 milligrams of pantothenic acid per day has been shown to produce some benefit for patients with osteoarthritis. However, a larger, better-controlled study failed to show any real benefit with pantothenic acid, even when the dosage was increased to 2 grams daily. Since most multiple-vitamin, multiple-mineral formulas provide at least 12.5 milligrams of pantothenic acid, additional supplementation doesn’t appear necessary, given its questionable benefit.

Vitamins A, B6, and E; Zinc, Boron, and Copper
These nutrients are required for the synthesis of normal col lagen and maintenance of cartilage structures. A deficiency of any one of these would allow accelerated joint degenera tion. Adequate intake of these nutrients can be achieved by taking a quality multiplevitamin, multiple-mineral formula that provides at least the RDA for these nutrients. Boron may not be included in some multiple-vitamin, multiple-mineral formulas, because no RDA for boron has been established. If the formula you take does not contain boron, take a supplement that provides you with 6 to 9 milligrams daily.
Typically, the standard American diet is severely deficient in fruits and vegetables, the major food sources of boron. Hence, many Americans’ intake of boron is insufficient. However, since the level of boron in foods is directly related to the level of boron in the soil, simply eating more fruits and vegetables may not be enough. Studies from a number of different countries have found that the lower the level of boron in the soil, the more often people develop osteoarthritis.
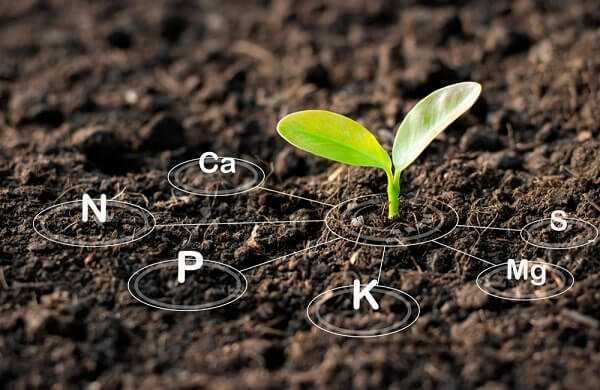
Boron supplementation has been used in the treatment of osteoarthritis in Germany since the mid 1970s. This use was recently evaluated in a small double-blind clinical study. Of the patients receiving 6 milligrams of boron (as sodium tetraborate decahydrate), 71% improved; only 10% in the placebo group improved. The preliminary indication is that boron supplements are of value in osteoarthritis treatment.
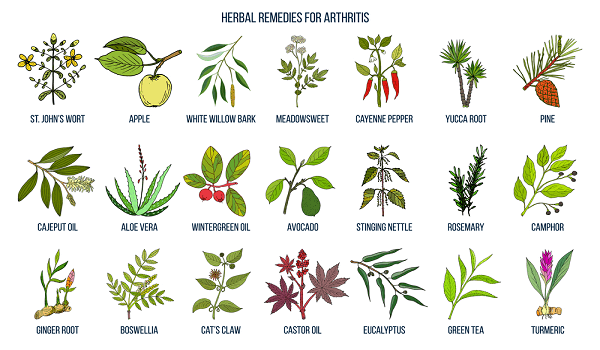
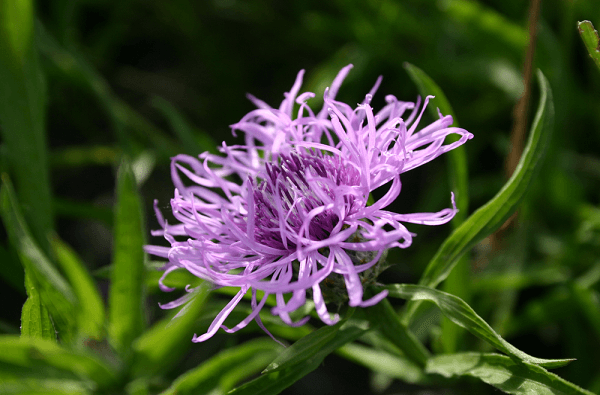
Plant-Based Medicines in Osteoarthritis Treatment
Many plants have been used in the treatment of osteoarthritis. If inflammation is present, botanicals and nutritional agents possessing anti-inflammatory activity are indicated. As inflammation is more of a factor in rheumatoid arthritis, natural anti-inflammatory substances are discussed in this article. Particularly useful are extracts of curcumin (a component of turmeric) and ginger.

In most cases of osteoarthritis, plant-based treatment addresses the underlying factors responsible for the degeneration. For example, plants rich in substances known as phytoestrogens are often used. These plant compounds are capable of binding to estrogen receptors on cartilage cells, thereby preventing the binding of the body’s own estrogen to the receptor. The higher prevalence of osteoarthritis in women suggests that estrogens may play a role. Experimental studies have demonstrated that estrogen promotes osteoarthritis. Several botanicals that have historically been used in the treatment of osteoarthritis are licorice root (Glycyrrhiza glabra) , dong quai (Angelica sinensis) , and alfalfa (Medicago sativa). Apparently they work by effectively blocking the negative effects of estrogen in osteoarthritis.

Although phytoestrogen-containing herbs are of value in treating osteoarthritis, perhaps the best way to increase their intake is to increase the intake of food that contains them. Food sources of phytoestrogens include fennel, celery, parsley, soy, nuts, whole grains, and apples. These foods, along with the regular consumption of alfalfa sprouts and licorice tea, will provide a much higher level of phytoestrogens than taking small amounts of herbs. Of course, if you are a menopausal woman, phytoestrogen herbs can be of tremendous benefit in dealing with the symptoms of menopause.
Boswellia
Another plant historically used in the treatment of osteoarthritis is Boswellia serrata, a large branching tree native to India. Boswellia yields an exudative gum resin known as salai guggul. Although salai guggul has been used for centuries, newer preparations concentrated for the active components (boswellic acids) are giving better results.

Boswellic acid extracts have demonstrated anti-arthritic effects in a variety of animal studies. There are several mechanisms of action, including inhibition of inflammatory mediators, prevention of decreased glycosaminoglycan synthesis, and improved blood supply to joint tissues. Clinical studies using plant-based formulas containing boswellia have yielded good results in osteoarthritis as well as rheumatoid arthritis treatment. The standard dosage for boswellic acids in arthritis is 400 milligrams, three times daily. No side effects due to boswellic acids have been reported.
Devil’s Claw
A plant native to Africa, devil’s claw (Harpagophytum procumbens) has a long history of use in the treatment of arthritis. Scientific studies of inflammation in animals show that devil’s claw causes an anti-inflammatory and analgesic effect comparable to that of the potent drug phenylbutazone Several clinical studies have also demonstrated some benefit. However, other studies have indicated that devil’s claw has little, if any, antiinflammatory activity.
The equivocal research results may reflect the mechanism of action of devil’s claw, which is inconsistent with that of current anti-inflammatory drugs, or it could reflect a lack of quality control (standardization) of the devil’s claw preparations used. Until these questions are answered, other natural measures should be used before trying devil’s claw in the treatment of osteoarthritis. At this time, devil’s claw appears to be better suited in the treatment of gout (see this article). Nonetheless, here are the recommendations in regard to devil’s claw.
Dosage (take these amounts, three times daily)
| Dried powdered root | 1 to 2 grams or as a cup of tea |
| Tincture (1:5) | 4 to 6 milliliters (1 to 1 ½ teaspoons) |
| Dry solid extract (3:1) | 400 milligrams |
Physical Therapy in Osteoarthritis Treatment
Various physical therapy treatments—exercise, heat, cold, diathermy, and ultrasound— performed by physical therapists, naturopathic physicians, and chiropractors are often very beneficial in improving joint mobility and reducing pain for sufferers of osteoarthritis. The importance of physical therapy appears to be quite significant, especially when administered regularly. Much of the benefit of physical therapy is thought to be a result of achieving the proper water content within the joint capsule, thereby facilitating the elimination of waste products and utilization of nutrients. Combining physical therapy measures—such as short-wave diathermy therapy with periodic ice massage, rest, and appropriate exercises—appears to be the most sensible approach.
Proper exercises include isometric exercises and swimming. These increase circulation to the joint and strengthen surrounding muscles without placing too much strain on the joint.
Final Comments
Although the primary treatment of osteoarthritis should consist of dietary therapy, nutritional and plant-based supplements can also be of exceptional value. Let me try and give some clear recommendations in terms of where to start with nutritional and plant-based supplements for osteoarthritis.
- Take a high-potency multiple-vitamin, multiple-mineral supplement that provides at least 100% of the RDA for all nutrients.
- Take an antioxidant supplement that will provide higher-than-RDA levels of some of the nutritional antioxidants, including vitamins C and E.
- Take glucosamine sulfate at a dose of 500 milligrams, three times daily.
Although further support is rarely necessary, the additional nutritional and plant-based supplements discussed in this chapter can be used if needed. Because the natural measures, such as glucosamine sulfate, may take up to a month or two to produce their benefit, some patients with severe osteoarthritis may need to continue with their NSAIDs. In this case, it is imperative to employ measures to protect the gastrointestinal tract from damage. Perhaps the best single recommendation is to use a special extract of licorice known as DGL, which is short for deglycyrrhizinated licorice. DGL has been shown to reduce the gastric bleeding caused by aspirin and other NSAIDs. DGL is strongly indicated for patients requiring long-term treatment with ulcer-causing drugs, such as NSAIDs and corticosteroids.
A history of NSAID or corticosteroid use is associated with peptic ulcers. Numerous studies over the years have found DGL to be an effective anti-ulcer compound. DGL’s mode of action is different than that of the current medications used for the treatment of peptic ulcers. Rather than inhibit the release of acid, licorice stimulates the normal defense mechanisms that prevent ulcer formation. Specifically DGL improves both the quality and quantity of the protective substances that line the intestinal tract, increases the lifespan of the intestinal cell, and improves blood supply to the intestinal lining.
DGL is superior to popular prescription drugs for ulcers. In several head-to-head comparison studies, DGL has been shown to be more effective than Tagamet, Zantac, or antacids in both short-term treatment of peptic ulcers and in consequent maintenance therapy. In addition, the drugs studied are associated with significant side effects, but DGL is extremely safe and is only a fraction of the cost. For example, Tagamet or Zantac typically costs well over $100 for a month’s supply. A month’s supply of DGL is available in health food stores for $15.

To be effective in healing or prevention, it appears that DGL must mix with saliva. DGL may promote the release of salivary compounds that stimulate the growth and regeneration of stomach and intestinal cells. The standard daily dose for DGL, in 380- milligram chewable tablets, is 2 to 4 tablets between, or 20 minutes before, meals. Continue using DGL for 8 to 16 weeks after stopping NSAID use. The DGL will help heal the damaged intestinal tract.