More about the Medical Aspects
Now that we’ve discussed the definition, diagnosis, and treatment of Sjogren’s syndrome, we know that you will still have specific questions about your individual symptoms and the way Sjogren’s affects you. This article is not meant to be a medical textbook with indepth information about every possible aspect of Sjogren’s, but we do want to provide explanations of certain potential symptoms and complications in greater detail.
Your Body and Sjogren’s
In this article, we examine how Sjogren’s can affect different parts of your body. We’ve organized the article so that you can scan it for the topics that especially interest you. Dry eyes and dry mouth are well covered in previous article, so we have gone into less detail here.
Your Eyes
Decreased tear production plus changes in tear quality contribute to eye symptoms in Sjogren’s syndrome. Three layers of tear film—aqueous, lipid, and mucin—make up the eye surface, and each one of them is affected in Sjogren’s.

Tearing decreases with age, which is why anyone without dry-eye disease can occasionally have eye discomfort. It is not normal, however, to develop a dry-eye state with persistent or frequent symptoms . We have already mentioned that many common medications can exacerbate dryness, but recently, investigators discovered that if you take hormones for menopause, your risk of dry eyes increases, although some women report just the opposite. If you are a woman who is older and taking hormone replacement therapy, your risk of dry eye is likely to be higher. According to a 2000 study at Schepens Eye Research Institute, 70 percent of women taking estrogen alone and 30 percent taking estrogen together with progesterone developed dry eyes. Low levels of the hormone androgen also contribute to dry eyes, and women have lower levels of androgen than men.
Your Mouth
We don’t often think about the joy of spit until we lose the ability to produce it. Unlike tears, saliva production does not naturally decrease because of age. Loss of saliva in Sjogren’s affects not only the mouth, as we’ve already discussed, but other areas of the body as well.

Your Salivary Glands
The major salivary glands are known as the parotid glands (the glands that begin under the ear and extend down the jaw and are commonly known as the “mump glands”). These glands are enlarged in one-third to one-half of people with Sjogren’s syndrome, changing the lines of your face and creating a slight chipmunklike appearance. The submandibular salivary glands, which lie under the jaw, can also become inflamed and swollen.
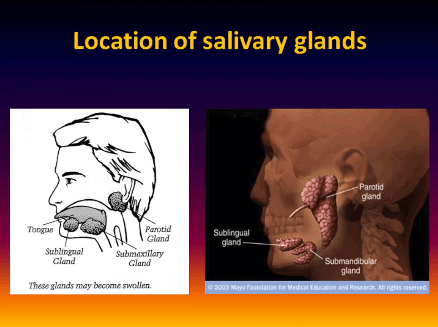
Swollen glands can be tender and painful, although not always. Acute pain sometimes signals infections which should be treated.
Recurrent swelling is not uncommon, but your doctor might want to check you for underlying complications if you have had prolonged swelling. Massive enlargement or hard, nodular glands can indicate onset of lymphoma and should be checked.
Your Ears
Dryness can cause itching in the ears. It can also affect the mucous glands of the eustachian tube, resulting in a feeling of stuffiness, muffled hearing, and middle ear infection.
Another potential for ear involvement in Sjogren’s is hearing loss. One recent study found 22.5 percent of Sjogren’s patients suffered from sensorineural hearing loss of cochlear origin. Autoimmune inner ear disease with resulting hearing loss can be considered an autoimmune disorder on its own, or it can accompany other autoimmune diseases such as Sjogren’s.
Tinnitus and potential hearing loss can be a side effect of certain medications. Aspirin can cause tinnitus, and hearing loss can be a rare side effect of the antimalarial drugs. If a new symptom appears while you are taking any drug, check the list of side effects and consult your doctor.
Your Nose
Dryness of the nasal and sinus passages can cause stuffiness and result in dry crusting and nosebleeds. The nerves and lining of the nasal passages can be damaged, reducing your sense of smell. This, in turn, can affect the taste of food.
Your Throat
The lack of saliva and the effect of Sjogren’s syndrome on the mucous membranes impact the throat, creating pain, complicating eating and digestion, and interfering with the vocal cords. Dryness can cause difficulty swallowing, and this can be complicated by lack of motility of the esophagus, atrophy of the mucous lining, and development of abnormal fibrous tissue in the throat. A dry larynx does not function as well as one that is moist, and dryness can make you hoarse. The continuous, dry cough common in Sjogren’s, or the need to cough up mucus from the throat, can contribute to sore throat and voice difficulties. Talking dries your mouth and throat further, making public speaking or talking for long periods on the telephone difficult.
Your Digestive System
Saliva aids digestion. From the moment food enters the mouth, the digestive process begins. Those with Sjogren’s syndrome are in trouble right from the start!
Mucous membranes that line the mouth and throat extend to the stomach and intestines. Atrophy and potential ulceration of these membranes complicates digestion, successful use of medications, absorption of nutrients, and the ability to fight infection.
Reflux, a common complication of Sjogren’s syndrome, contributes to irritation and damage of the esophagus.
Your Pancreas
Sjogren’s syndrome can affect the production of digestive enzymes by the pancreas, further complicating digestion. The pancreas can also become inflamed in Sjogren’s, a condition called pancreatitis, although this is unusual. Pancreatitis is marked by abdominal pain and increased levels of amylase, a pancreatic enzyme, but because this enzyme is often elevated in someone with Sjogren’s, you will need to distinguish whether the increased amylase is of pancreatic or salivary gland origin.
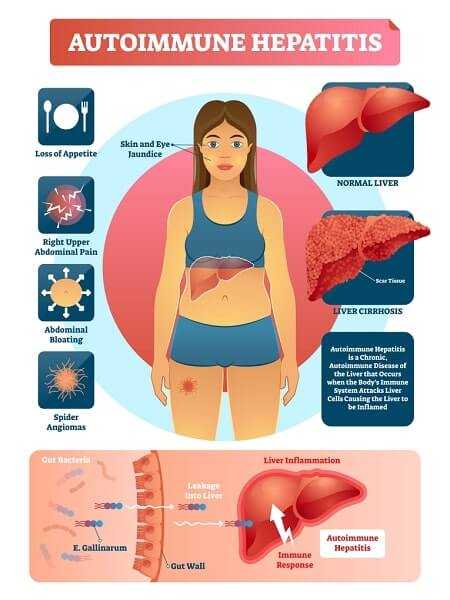
Your Liver
Researchers report frequent abnormal liver findings (liver function or enlargement) in Sjogren’s patients, although researchers’ percentages vary widely from 25 percent to 58 percent. If you have abnormal findings, this does not always mean you have liver disease, but it shows once again how Sjogren’s can frequently affect many organs. Two autoimmune liver diseases are associated with Sjogren’s, primary biliary cirrhosis and autoimmune hepatitis.
Primary Biliary Cirrhosis
Primary biliary cirrhosis (PBC) is the liver condition most closely connected with Sjogren’s. About 70 percent of those with this autoimmune liver condition have symptoms of Sjogren’s syndrome More about the Medical Aspects 49, and about 10 percent of those with Sjogren’s have PBC. The main symptoms are itching all over your body and fatigue. PBC causes progressive liver damage and can remain mild or lead to liver failure.

Autoimmune Hepatitis
Autoimmune hepatitis means inflammation of the liver, and inflammation is caused by autoantibodies. The condition can be treated with corticosteroids. Untreated autoimmune hepatitis can lead to cirrhosis, or hardening of the liver, and liver damage.
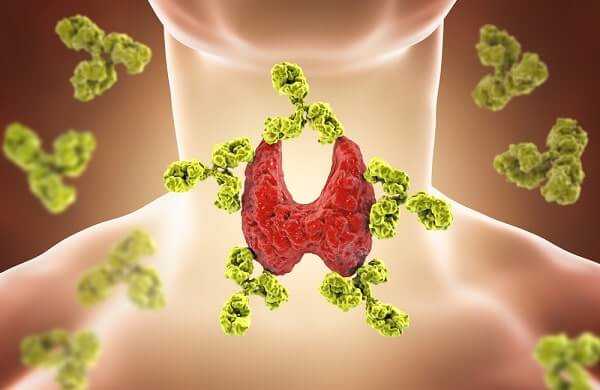
Your Thyroid
Autoimmune thyroid conditions are commonly found in those with Sjogren’s or in family members of someone with Sjogren’s. Almost 30 percent of Sjogren’s patients have thyroid gland dysfunction or thyroid antibodies. The thyroid, a small gland just below your Adam’s apple, regulates your metabolism. It does this by producing thyroid hormones. In autoimmune disease, specific autoantibodies can cause your thyroid to either overproduce (resulting in Graves’ disease) or underproduce (resulting in Hashimoto’s thyroiditis) these hormones.
Many of the symptoms of autoimmune thyroid conditions can be confused with symptoms you might already be experiencing from Sjogren’s. A simple blood test for hormone levels will provide you and your physician with a quick answer. Your doctor might also test for thyroid antibodies.
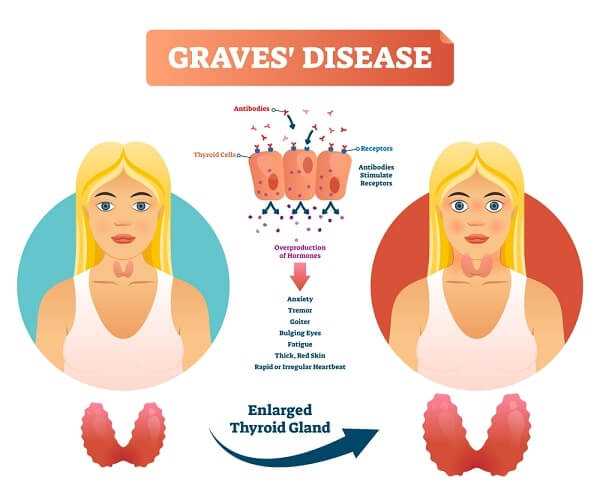
Graves’ Disease
If you have Graves’ disease, your thyroid is hyperactive, meaning you produce too much thyroid hormone. Graves’ is known for sometimes causing a bug-eyed look, where your eyes seem to protrude. Your eyes can become inflamed and surrounding tissue swollen. Other signs can include weight loss, a hot and flushed appearance, fast or irregular pulse, muscle weakness, and lighter and less frequent menstrual periods. Graves’ can also cause nervousness, irritability, hair loss, and dry hair and nails. Thyroid hormone levels will need to be checked every year because they can change and medication might need to be adjusted.
Hashimoto’s Thyroiditis
If you have Hashimoto’s thyroiditis, your thyroid tends to be underactive, meaning you produce too little thyroid hormone. An underactive thyroid can cause you to gain weight; feel cold, sluggish, and depressed; develop a slow heart rate, muscle cramps, dry and brittle hair, and itchy skin; and have heavier menstrual periods.
Your Lungs
Dryness of the lungs and upper respiratory tract and inflammation of the bronchial glands can lead to bronchitis and recurrent pneumonia. A dry cough is common. You can have difficulty breathing and pain with breathing. Fibrosis, or scarring, of the lung can occur, leading to interstitial pulmonary fibrosis. White blood cells, or lymphocytes, might invade the lung tissue just as they might invade any organ or tissue in the body in autoimmune disease. This lymphocytic infiltration can lead to development of malignant lymphoma, which can sometimes occur in the lungs in those with Sjogren’s (accounting for about 20 percent of the lymphomas in Sjogren’s).
Your Joints and Muscles
Joint and muscle pains are common symptoms of rheumatic diseases, and Sjogren’s syndrome is no exception. Symptoms can include stiffness and pain, especially in the morning.
Your Nervous System
Involvement of your peripheral nervous system (PNS)—that is, the nerves throughout your body excluding the brain and the spinal cord—is not uncommon in Sjogren’s syndrome. Antibodies can attack the nerves or blood vessels causing inflammation, and when blood flow to the nerves is impaired, nerve damage can result. For most Sjogren’s patients who experience nervous system involvement, the condition is mild and not debilitating.
Your Peripheral Nervous System
Involvement of the PNS usually causes abnormal sensations and primarily affects your legs and feet, and less frequently, your hands and arms. This sensory nerve involvement can lead to decreased sensation, sometimes referred to as a “stocking and glove” sensation and described as tingling, burning, and feeling like pins and needles. You also might have severe pain.
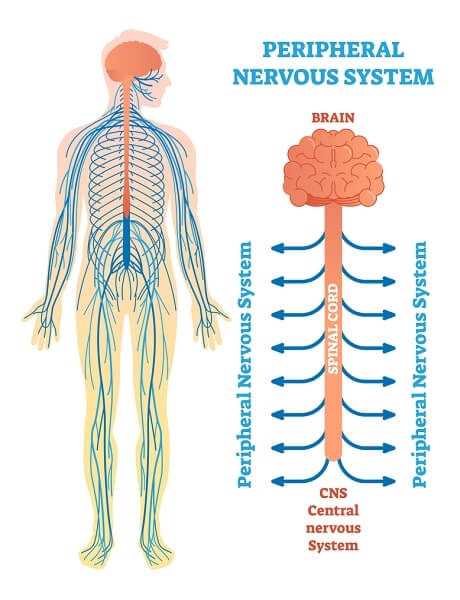
PNS involvement can also affect the cranial nerves, which can become inflamed and cause tingling in the scalp and head and headache, and affect your sense of taste and smell and even your eyesight. A condition called trigeminal neuralgia, the most common cranial nerve involvement, can cause facial numbness and pain and even make the surface of your eyeballs numb.
Another common type of PNS involvement is entrapment neuropathy, in which a nerve becomes numb because it’s “trapped” or compressed. Carpal tunnel syndrome is a common example. In this syndrome, the wrist and hand become numb when the median nerve is compressed, or trapped by swollen tissue. Another example is tarsal tunnel syndrome, which causes burning and pain in the bottoms of your feet when walking or cycling.
Motor nerves are infrequently involved, but when they are involved, motor activities, including walking, balance, and manual dexterity can be affected.
The autonomic nervous system is part of your peripheral nervous system and includes nerves controlling involuntary or semi-voluntary nerve actions. Involvement of the autonomic nervous system can cause decreased sweating, affect your ability to regulate body temperature, contribute to decreased tears and saliva and difficulty swallowing, cause dizziness, and involve the bowel and bladder and result in incontinence.
Peripheral nerve involvement is often marked by periodic and spontaneous improvement, so unless the pain or numbness is extreme, further testing or treatment probably will not be offered. Electrophysiologic studies (such as electromyography and nerve conduction tests) can determine the extent of damage to peripheral nerves, but these tests will only pick up on major damage. Most people with peripheral neuropathy test positive for the autoantibody SSA.
Your Central Nervous System
The brain and spinal cord make up the central nervous system (CNS). CNS involvement in Sjogren’s syndrome clearly occurs in some patients, although the extent of the problem in Sjogren’s remains controversial. While CNS involvement in lupus became well-established long before that in Sjogren’s syndrome, a group at Johns Hopkins finally brought the Sjogren’s-CNS connection to the fore in the 1980s, and studies continue to emerge in this interesting area.
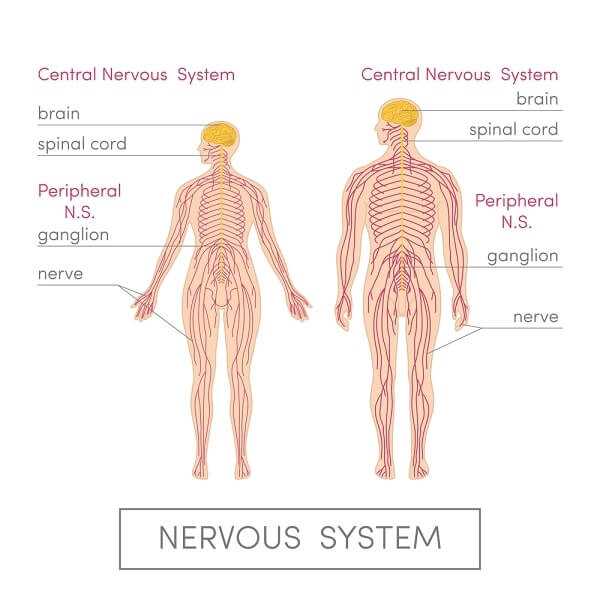
CNS involvement in Sjogren’s can resemble multiple sclerosis, and your neurological symptoms in Sjogren’s can mimic or be misdiagnosed as multiple sclerosis. You might develop cognitive dysfunction, including problems with memory and concentration.
If your doctor suspects CNS involvement, he or she will probably order a brain MRI, which can show evidence of white matter—or spots of signal intensity—and perhaps test your spinal fluid. Many other tests that provide greater information about the brain and spinal cord, such as electrophysiologic studies, cerebrospinal fluid analysis, and cerebral angiography, might only be offered at major medical centers. Until you experience multiple or severe and damaging events of CNS, treatment is often conservative and physicians prefer to keep a close watch. If you do need treatment, powerful immunosuppressive therapy, administered intravenously and usually by a method called pulse therapy (given intermittently), is successful and problems can even be reversed. The immunosuppressives of choice in this case are corticosteroids or cyclophosphamide.
Your Vascular System
The nervous and vascular systems are closely interrelated, so if you have neuropathy (a disease of the nerves), you might also have vasculitis, which is inflammation of your blood vessels. Vasculitis in Sjogren’s syndrome is usually restricted to the small blood vessels, where immune complexes and antibodies cause inflammation and destruction. This process can impact many organs, because if blood flow does not reach tissues, the tissue can be damaged and organ function affected. If medium-size arteries are affected, blood flow to the fingers and toes can be reduced, leading to tissue death, or gangrene.
Capillaries that are destroyed can cause blood to leak just under the skin. This can show up as reddish purple spots, or purpura. Small hemorrhaging can lead to small red spots called petechiae.
Antiphospholipid Antibody Syndrome
In antiphospholipid antibody syndrome (APLS), autoantibodies to phospholipids (a type of fat) increase your risk of blood clots. If you have APLS, you are at increased risk for deep vein thrombosis, stroke, heart attack, and pulmonary embolism (when a blood clot travels to the lungs). APLS can cause miscarriages, so if you’re trying to become pregnant, it’s important to be tested for this syndrome.
Nearly 5 percent of primary Sjogren’s patients and 13 percent of secondary Sjogren’s patients have APLS. The syndrome is not associated with an increased incidence of central nervous system involvement in Sjogren’s . However, if you have both APLS and the autoantibody SSA, your chances of developing vascular disease increases.
APLS will be diagnosed if you have both anticardiolipin antibodies and the lupus anticoagulant in conjunction with episodes related to blood clotting, together with problems such as miscarriages, strokes, and heart murmers.
Raynaud’s Phenomenon or Disease
Cold can cause blood vessels to constrict, reducing blood flow and turning fingers red, white, and blue. Ulceration can occur. This condition can be called either Raynaud’s phenomenon or Raynaud’s disease, depending on its severity. Raynaud’s is frequently associated with Sjogren’s as well as other autoimmune disorders.
Your Skin
Dry, flaky skin is a common feature of Sjogren’s. Dryness leads to itching, which can get worse in the winter with dry air. Scratching can lead to infection.

You might develop hives or rashes. Reaction to sunlight, especially evident in patients positive for the antinuclear antibody SSA, can result in a rash. If you have a butterflyshaped rash across your nose and cheeks, your doctor will suspect lupus.
The skin’s appearance reflects many autoimmune complications. If you have Raynaud’s, your fingers change color. In vasculitis, red and purple spots appear, especially on extremities, and autoimmune liver disease causes a yellowish cast to the skin all over your body. If you suffer from scleroderma along with your Sjogren’s, you can develop rough, hardened skin and your skin can lose its elasticity.
Your Hair
Hair can be dry, brittle, and dull in Sjogren’s. Hair loss can occur with autoimmune diseases, including Sjogren’s, a condition known as alopecia. Hair loss can also occur in the autoimmune thyroid disorder. Graves’ disease.
Your Heart
Heart problems are unusual in Sjogren’s syndrome and are more often correlated with lupus. Sjogren’s and lupus are closely associated, however, and heart problems can, indeed, occur. Just as inflammation of the lung lining can take place, inflammation can affect the lining of the heart. This condition is called pericarditis. In addition, irregular and slow or fast heart rates can occur with autoimmune thyroid disorders.
Your Kidneys
Just like other organs, the kidneys can become inflamed in Sjogren’s syndrome, leading to interstitial nephritis. This type of inflammation makes it difficult to produce concentrated urine, so you urinate more frequently and in greater volume. Renal tubular acidosis can also occur and lead to potassium depletion. A third and rarer kidney complication in Sjogren’s is glomerulonephritis, which is more commonly found in lupus.
How do you know you have kidney complications? People often think of lower back pain as being connected with the kidneys, but this symptom is not found in autoimmune kidney disorders. Most likely you would have no symptoms, although you might experience swollen ankles and a feeling of abdominal bloating. Evidence usually starts with abnormal urinary and blood tests. Your urinalysis might show excess protein, called proteinuria; blood urea nitrogen (BUN) and creatinine levels can also point to a potential kidney problem.
Your Bladder
Urinary complaints are not uncommon in Sjogren’s syndrome We all know that drinking liquids throughout the day and night leads to numerous trips to the bathroom and disruption of sleep. Bladder irritation can occur and bladder inflammation sometimes accompanies Sjogren’s. Urinary frequency, urgency, and pain can ensue.
Your Reproductive System
Moisture production in the vaginal area is frequently depleted in Sjogren’s, affecting the health of the vaginal tissues and causing an increased tendency for developing infection and experiencing pain during intercourse.
Planning a pregnancy with Sjogren’s syndrome requires some special considerations:
- Are you taking medications that might interfere with your becoming pregnant or that you will have to stop taking if you should become pregnant?
- Do you have an antiphospholipid antibody that could interfere with a pregnancy?
- If you have anti-SSA and/or anti-SSB antibodies, have you talked with your doctor about the possibility of complete heart block (a complication that occurs in babies born to mothers with these antibodies)? In heart block, an abnormally low heart beat is detected between twenty and thirty weeks of gestation. This cardiac problem develops because the normal electrical signals that regulate fetal heartbeat are interrupted by the mother’s autoantibodies.
Hormone changes in pregnancy can impact the autoimmune disease process in the mother. Sometimes the change is for the better—many women say their Sjogren’s syndrome improves during pregnancy. Sometimes the change is for the worse; some women report flare-ups during the roller coaster changes in hormones. You and your doctor will have to determine which medications you can continue during pregnancy and weigh your need for disease control with the potential impact of medications on the fetus.
Is it safe to take hormone replacement therapy for menopause or hormones for birth control? We don’t know. Studies have shown contradictory results and this topic continues to be hotly debated. Because estrogen is known to cause flare-ups in autoimmune disease, some doctors recommend avoiding it. Many studies have shown hormone replacement therapy to help prevent osteoporosis and cardiovascular problems, so if you are at risk for these problems, you and your doctor might lean toward using this therapy. Recent studies question these benefits, however. More studies are desperately needed.