Drugs Used in the Early Stage of Alzheimer Dementia

The first manifestation of Alzheimer dementia is often memory disturbance. Therefore, attempts to treat the early stages of this disease are frequently directed at the improvement of memory function and other cognitive deficits. In addition to cognitive problems, many patients also exhibit mood and personality changes in the early stages of the illness. Drugs affecting mood (antidepressants) are frequently employed in the early stages of Alzheimer dementia, although they do not directly affect the dementing process.
Ergoloid Mesylates
A mixture of ergoloid mesylates (Hydergine, Niloric) is the only drug preparation that has been shown to be effective in improving the cognitive performance of patients with earlystage dementia and that is available for this use in the United States. Ergoloid mesylates are extracted from ergot. Their chemical structure is quite complex and includes a tryptamine-like portion that is similar to the neurotransmitter serotonin. Ergoloid mesylates affect several neurotransmitter systems in the brain. In animal experiments, they have been shown to act as norepinephrine antagonists and to decrease production of cyclic adenosine monophosphate and of sodium-potassium-dependent adenosine triphosphatase activity. Ergoloid mesylates also block the effects of dopamine and serotonin and increase choline acetyltransferase activity in the brains of aged animals. In humans, ergoloid mesylates increase fast electroencephalographic activity without any significant effect on the cerebral blood flow. It is not clear which of these mechanisms is responsible for the beneficial effects of ergoloid mesylates observed in patients with dementia.

In controlled clinical trials, ergoloid mesylates were found to improve some symptoms of dementia in elderly patients, including decreased alertness, confusion, emotional lability, and bothersomeness. However, in most of these studies different types of dementia were not differentiated, so it is not certain that these effects would occur in Alzheimer patients. Ergoloid mesylates have been approved bv the Food and Drug Administration (FDA) for use in idiopathic decline of mental capacity but not for a specific disease. One of the few studies of ergoloid mesylates specifically directed to patients with Alzheimer dementia was conducted in several Veterans Administration medical centers. In this study the effect of ergoloid mesylates on intellectual and emotional functioning in mildly demented patients was compared with desipramine, thiothixene, and placebo using several standardized rating scales. The only significant difference between ergoloid mesylates and placebo was on the Pervasive Affective Disturbance Scale of the Zung Symptom Checklist in which patients receiving ergoloid mesylates performed worse than patients receiving placebo. On other scales, patients on ergoloid mesylates were rated better than patients on the other two medications, but there was no significant difference from the placebo. On the History of Psychic and Somatic Complaints in Elderly Scale patients on ergoloid mesylates were rated worse than patients on desipramine or thiothixene. Thus, it is possible that ergoloid mesylates do improve cognitive performance of Alzheimer patients somewhat but, at the same time, increase their complaints.
Treatment with the mixture of ergoloid mesylates is relatively safe. The most significant adverse effect is an orthostatic hypotension, which might lead to dizziness, fainting spells, and falls. With sublingual administration of ergoloid mesylates some irritation of the mouth, transient nausea, and gastric disturbances have also been reported. Since the mixture of ergoloid mesylates is the only medication currently available for the treatment of cognitive symptoms in Alzheimer dementia and because it is relatively safe, many physicians routinely use it in early stage dementia. It has also been reported that ergoloid mesylates inhibit platelet aggregation. This could decrease the progression of multiinfarct dementia, which sometimes coexists with Alzheimer dementia and may be difficult to distinguish from it.
Vasodilators
The earliest approach to the drug treatment of dementia was based on the hypothesis that dementia occurs in older people because the blood supply to the brain is compromised by aging-induced ”hardening of the arteries.” In 1780, the American physician Dr. Benjamin Rush used a rotating chair in which elderly demented patients were strapped and spun around. He reasoned that the centrifugal force would increase blood flow to the brain and improve brain function. A similar hypothesis, but with a somewhat more modern technology, was the basis of a therapy introduced in the 1920s. Patients with dementia were placed in a hyperbaric chamber in an attempt to increase oxygen supply to the brain and improve cognitive function. Needless to say, neither the rotating chair nor the hyperbaric chamber is effective in the treatment of dementia.
Based on the vascular hypothesis, a whole class of drugs was developed and tested for the treatment of dementia. These drugs, vasodilators, were supposed to dilate brain blood vessels and thus increase the oxygen supply to the brain. The vasodilator drugs include papaverine (Pavabid, Cerespan), cyclandalate (Cy-clospasmol), isoxsuprine, nylidrin, niacin derivatives, and some other agents that are not available in the United States. When studied by rigorous double-blind techniques, however, most of these drugs were found to be ineffective in improving the symptoms of dementia. An exception is nafronyl, which was found to be somewhat effective in improving cognitive function and is used abroad in patients with Alzheimer dementia. Its effectiveness is similar to that of the ergoloid mesylate mixture, which was also originally developed as a vasodilator. Neither nafronyl nor ergoloid mesylates, however, improve dementia symptoms by producing vasodilation. According to our current understanding, the blood supply to the brain in Alzheimer patients is intact. Although oxygen consumption in the brain is lower in Alzheimer patients than in controls, this decrease is a consequence of brain cell death and brain atrophy rather than a cause for degeneration of the brain.
Multi- infarct dementia, on the other hand, is believed to be a consequence of cerebrovascular disease. Even in this form of dementia, however, vasodilation would not be beneficial for the regions of the brain supplied by pathologically constricted blood vessels. Vasodilators do not increase blood flow in a blood vessel that is narrowed by an atherosclerotic process, because such a vessel is rigid and cannot be dilated effectively. In fact, since it is the normal vessel that will dilate after administration of vasodilators, the blood is siphoned off through dilated normal blood vessels away from the cerebral regions that are supplied by pathologically constricted blood vessels (so-called steal effect). Therefore, vasodilation may actually worsen symptoms in some patients with cerebral atherosclerosis.
Blood flow measurements indicate that nafronyl actually does not increase blood flow to the brain. It may produce its beneficial effect by directly influencing cerebral metabolism because it increases the pyruvate/lactate ratio in cerebrospinal fluid and fast electroencephalographic activity. However, its exact mechanism of action is unknown.
Cholinergic Drugs
Several lines of evidence indicate that the cholinergic system in the brain is abnormal in Alzheimer dementia. This system, whose neurotransmitter is acetylcholine, regulates a variety of brain functions, including memory processes. Activity of the enzyme choline acetyltransferase, which synthesizes acetylcholine from choline and acetate, is markedly decreased in postmortem brain tissue or biopsy specimens taken from Alzheimer patients. Postmortem investigation also shows that the number of cholinergic nerve cells in the basal forebrain of Alzheimer patients is markedly smaller than in nondemented people of the same age. This is true especially in patients with onset of dementia before the age of 65. In addition, drugs that impede the cholinergic activity by blocking cholinergic receptors produce temporary memory disorders in normal people. It is not clear, however, that the memory disturbance induced by these drugs is the same as that observed in Alzheimer dementia.
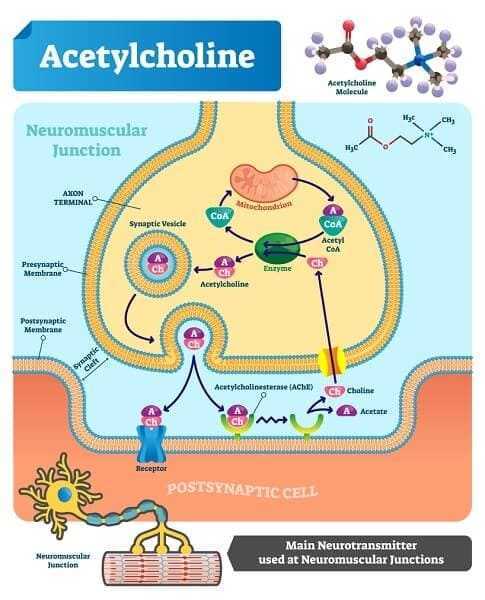
Considering this information, it might be predicted that increasing central cholinergic activity would be beneficial in Alzheimer’s disease. There are three strategies that could be used in an attempt to increase cholinergic activity. These include administration of acetylcholine precursors, the use of drugs that stimulate acetylcholine receptors, and administration of drugs that inhibit acetylcholine metabolism.
Acetylcholine Precursors
Animal experiments have shown that oral or parenteral administration of choline increases acetylcholine levels in the brain. Based on this information, many investigators have attempted to improve cognitive function in Alzheimer patients by oral administration of choline-containing lecithin. This strategy is similar to that used in treatment of Parkinson’s disease, a condition in which a biochemical deficit of the neurotransmitter dopamine can be corrected by the administration of the dopamine precursor levodopa.
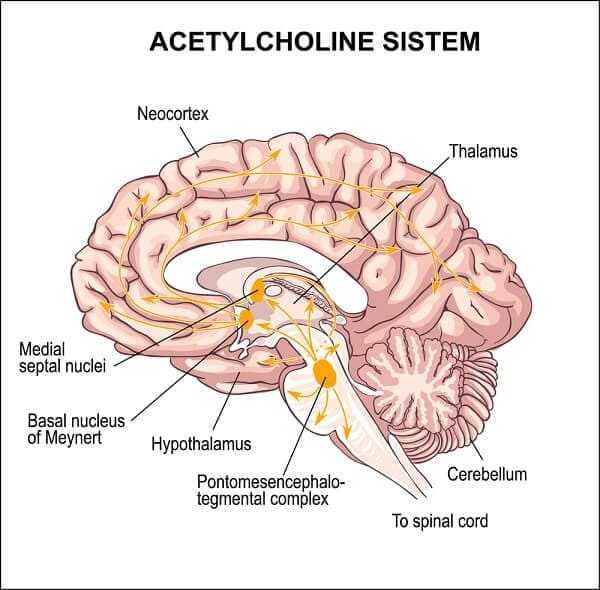
Although different doses of lecithin have been investigated in the treatment of Alzheimer dementia and, in some cases, the trials were continued for a long time period, no significant effects of acetylcholine precursors on memory processes have been observed. It is possible that although the administration of lecithin does increase acetylcholine synthesis, it does not increase the physiologic release of acetylcholine from cholinergic nerve endings. In contrast to the dopaminergic system, which provides tonic inhibition to the basal ganglia, the cholinergic system provides selective stimulation of distinct brain areas. Therefore, a general increase in acetylcholine levels might not improve selective acetylcholine release. Alternatively, since acetylcholine is only one of several neurotransmitters affected by the Alzheimer dementia, an isolated improvement of the cholinergic function might not lead to significant clinical improvement.
Cholinergic stimulants
Central cholinergic activity could also be influenced by the administration of drugs that directly stimulate cholinergic receptors. Again, this strategy is similar to one form of treatment of Parkinson’s disease in which dopaminergic agonists (e.g., bromocriptine) are quite effective. Systemic administration of cholinergic agonists, however, leads to cholinergic stimulation of peripheral organs and to undesirable side effects such as diarrhea, abdominal cramping, and bradycardia. The direct administration of cholinergic agonists into the brain appears to be more promising because it would lead to fewer side effects.
Harbaugh and co-workers implanted a pump that injected a cholinergic agonist, bethanechol, directly into the cerebral ventricles of Alzheimer patients. They reported some improvement in some patients with minimal side effects. However, the patients were evaluated only subjectively and no objective ratings were performed. The value of this method for treatment of Alzheimer dementia will have to be evaluated on larger numbers of patients using objective rating scales.
Acetylcholine Esterase Inhibitors
Acetylcholine esterase is an enzyme that terminates the action of acetylcholine released from nerve endings by breaking it down into choline and acetate. The first acetylcholine esterase inhibitor to be investigated in Alzheimer dementia was physostigmine (Antilirium). Intravenous administration of this drug improved memory in normal volunteers and also in some Alzheimer patients. However, intravenous administration is not practical for long-term management. Treatment with oral physostigmine improved cognitive function in some Alzheimer patients but even in those individuals the effect of physostigmine was quite small and only temporary. The use of physostigmine has two major disadvantages. The drug has a short duration of action and has to be administered every 2 to 4 hours to produce sustained inhibition of acetylcholine esterase. In addition, physostigmine potentiates cholinergic activity not only in the brain but also in peripheral organs and this results in a high incidence of side effects, such as diarrhea, abdominal cramps, and bradycardia.
An effort has been made to develop and test other acetylcholine esterase inhibitors that might be more selective for the brain acetylcholine esterase. A pronounced improvement of cognitive function in Alzheimer patients who received tetra-hydroaminoacridine (THA) has been reported. This inhibitor caused relatively few side effects and was most effective in early stage Alzheimer patients. Unfortunately, limited long-term follow-up indicated that the effectiveness was not sustained with time. Such a result might be predicted since inhibition of cholinesterase activity does not affect the basic degenerative process of Alzheimer dementia leading to progressive loss of cholinergic neurons. Since inhibition of cholinesterase merely potentiates existing cholinergic activity, its effectiveness will be lost when cholinergic neurons disappear. Recently, a large-scale trial of THA had to be terminated because the drug caused liver damage.
Antidepressants
The incidence of depression in patients with dementia of Alzheimer type is not clear. It is difficult to diagnose depression in a demented patient because many symptoms of major depressive disorders are similar to those of Alzheimer’s disease (e.g., sleep disturbance, fatigue, psychomotor agitation or retardation, loss of interest in usual activities, and diminished ability to think or concentrate). The major criterion, depressed mood, may be difficult to assess by subjective report because of poor motivation to report, loss of affect recognition, or aphasic difficulties.
Estimates of coexistent depression in dementia vary widely, from 15% to 57%. Since many authors do not mention how they resolved the diagnostic dilemma, it is difficult to interpret these reports. Another issue concerns whether dementia can be caused by depression. Some authors refer to a “pseudodementia,” as a main symptom of depression in older people. However, even in elderly patients who improve following antidepressant treatment, the follow-up indicates that many of them later develop a classic picture of progressive Alzheimer dementia.
There is no agreement concerning the use of antidepressants in the treatment of Alzheimer dementia. Reisberg mentions “mourning” following insight into the illness and “blunting” of the emotions but does not recommend treatment. On the other hand, Reifler and co-workers, who found depression in 31% of their patients, report that treatment led to improvement in mood, vegetative signs, and activities of daily living in 85% of these patients. The potential benefits of antidepressant therapy have to be balanced with the possibility of side effects induced by antidepressants, which include life-threatening cardiovascular complications. Since the prognosis of Alzheimer dementia is unfortunately poor, however, it may be reasonable to risk possible side effects of antidepressant treatment in order to exclude treatable depression as a possible underlying cause of the disturbed mental state.

Many drugs exhibit antidepressant activity. According to their mechanism of action, they can be divided into inhibitors of monoamine oxidase (e.g., tranylcypromine [Parnate]) and inhibitors of norepinephrine and/or serotonin reuptake (e.g., imipramine [Tofranil], amitriptyline [Elavil], doxepin [Sinequan], nortriptyline [Pamelor], amoxapine [Asendin], nomifensine [Merital]). Both classes act by potentiating the effect of norepinephrine or serotonin, either by blocking their metabolism (inhibitors of monoamine oxidase) or by prolonging their action on the receptors (inhibitors of reuptake).
Most inhibitors of reuptake block the reuptake of both serotonin and norepinephrine, but to a different degree. These agents also affect other receptors, mainly muscarinic and histamine receptors. This leads to two most common side effects: anticholinergic effects and sedation. Anticholinergic effects include blurred vision, dry mouth, sinus tachycardia, constipation, urinary retention, increased intraocular pressure, and worsening of memory function. One classic and two newer antidepressants will be described in more detail.
Desipramine
Desipramine (Norpramin) is a representative of the most commonly used “tricyclic” antidepressants, named according to their chemical structure. Desipramine predominantly blocks norepinephrine reuptake and has a much smaller effect on serotonin reuptake. Desipramine does not have a strong anticholinergic activity and produces less sedation than other antidepressants. It is metabolized by hydroxylation in the liver, and this process is decreased by cimetidine (Tagamet) but not by aging.
Administration of desipramine poses a risk to patients with cardiovascular or thyroid disease because of the possibility of an arrhythmia or acute myocardial infarction (although this risk is lower than with other tricyclic antidepressants). It also poses a problem for patients with a history of urinary retention or glaucoma, because of the anticholinergic activity, and for patients with a history of seizure disorder, because desipramine lowers the seizure threshold. Patients should be warned that while taking desipramine they might be more sensitive to the effects of alcoholic beverages. The therapeutic effect of desipramine may be seen after 2 to 5 days, but full effect usually requires continuation of treatment for 2 to 3 weeks.
Maprotiline
Maprotiline (Ludiomil) has a four-ring chemical structure instead of the three-ring structure characteristic of most other antidepressants. It also preferentially inhibits the reuptake of norepinephrine, and its metabolism is inhibited by cimeti-dine (Tagamet). Maprotiline has fewer anticholinergic side effects than other antidepressants, and it has been used successfully in patients who developed acute urinary retention during treatment with other antidepressants. It is also effective in decreasing anxiety but produces more sedation than desipramine.
Maprotiline should be also given with caution to patients with cardiovascular or thyroid disease, because of the possibility of arrhythmias and acute myocardial infarction, and to patients with history of seizures, because it lowers seizure threshold. The development of seizures is more likely if the patient is being treated simultaneously with a neuroleptic drug (e.g., haloperidol [Haldol]), or if benzodiazepine therapy has been recently discontinued. Reports that maprotiline has an earlier therapeutic effect than other antidepressants have not been confirmed by subsequent studies.
Trazodone
Trazodone (Desyrel) is a triazolopyridine derivative unrelated to the other antidepressants. Its main action is on the serotoninergic system. It blocks both serotonin reuptake and serotonin receptors. Trazodone is metabolized by hydroxylation in the liver, and this process is inhibited by cimetidine (Tagamet). It does not have any anticholinergic activity but produces sedation, dizziness, hypotension, and cardiac arrhythmias with a frequency similar to that of the other antidepressants. One of its more serious side effects, discovered after it was used for several years, is the development of priapism, a prolonged, painful penile erection that, in some cases, requires surgical treatment and may lead to permanent impotence.

Trazodone has been reported to improve assaultive behavior in patients with organic brain syndrome, including Alzheimer dementia. In the four patients described, the clinical presentation did not suggest a primary depressive illness and neuroleptics were ineffective in controlling the symptoms. Trazodone is effective in decreasing aggressive behavior in some animal models, and it is possible that its effect on the serotoninergic system mediates this activity.
Aspirin
The diagnosis of Alzheimer dementia is made by exclusion of other causes of dementia. However, distinguishing the clinical features of other causes of dementia from those of Alzheimer dementia may be difficult. This is especially true for multiinfarct dementia, which is caused by repeated occlusions of small blood vessels in the brain. Furthermore, Alzheimer dementia and multi-infarct dementia are often combined, and in one third of demented patients both infarcts and Alzheimer changes were found at autopsy. It is unclear which of these changes are more important for the clinical syndrome of dementia.

Therefore, it is important to consider the possibility that a patient diagnosed as having Alzheimer dementia may also have multi-infarct dementia. Drugs that inhibit platelet aggregation, (aspirin) may prevent further occlusion of cerebral vessels. Small doses of aspirin are optimal for inhibition of production of thromboxane, which promotes platelet aggregation, without decreasing the production of prostacyclin, which inhibits platelet aggregation and dilates blood vessels. Thus, either one children’s aspirin (65 mg) every day or a regular aspirin (325 mg) every other day might be beneficial in patients with dementia by decreasing the probability of further infarcts.