A Cheat Sheet for Coping with Rheumatoid Arthritis Flares

It may seem as if flares are the most difficult tests of all to endure. Every time I experience a flare, I think that I know what to expect but regardless of experience, it seems that every flare is different.

Yet, in some ways, they are all the same. In the moments where I feel a great deal of pain, the fatigue is at its worst and I am extremely overwhelmed, it is hard to have a clear perspective. What I have found, however, is that having a plan, or a cheat sheet, for dealing with a flare makes coping so much easier.
What ignites a flare?
What we all know about rheumatoid arthritis (RA) flare-ups is that they are unpredictable. Sometimes they come often, and other times you can enjoy longer periods of remission with only sporadic attacks of inflammation and fatigue. A flare can occur in few joints or it can affect the whole body, and it can last for days or even weeks.
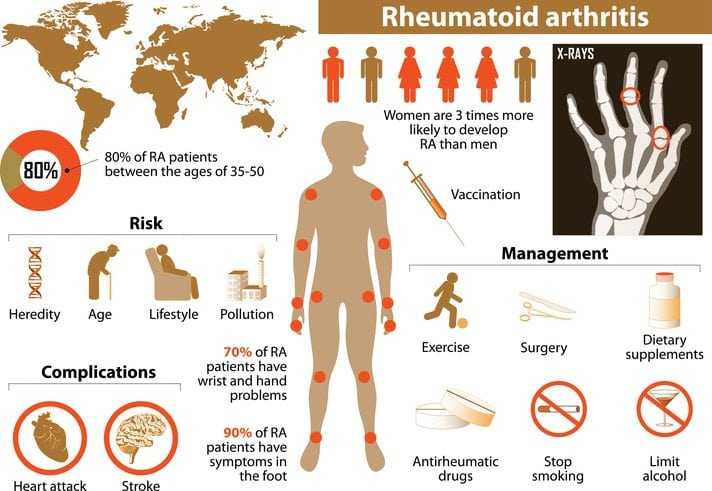
Any number of things can trigger flares and they are not necessary specific to certain foods, hormones or even stress. Other factors that can ignite flares include smoking and the weather. That is why it is so important to educate yourself on living with RA and dealing with its effects. Further, being informed allows you to quickly evaluate an oncoming flare and to work towards coping through it successfully.
My cheat sheet for coping
I have a yellow post-it note in my medicine cabinet (taped to the inside part of the door) that has the following written on it: “For Flares: No drugs, rest and exercise, watch what you eat, try alternative therapies, drug options and call your doctor.” When a flare happens, I try to follow these in order depending on the severity of the flare, and then continue them throughout the duration of the flare.
Here my cheat sheets tips for coping with a flare:
Start with No Drugs. The reason I keep my cheat sheet in my medicine cabinet is to remind myself to consider non-drug therapies before medicinal approaches. Heating pads and cold packs can be applied to affected areas to reduce pain and swelling.
Doctors recommend resting affected joints and applying ice for 20 minutes on and 20 minutes off for a period of two hours. Alternate between hot and cold every two hours with the same schedule – 20 minutes on and 20 minutes off.

Alternate Between Rest and Exercise. We know that rest is essential during a flare period, but so is exercise. This is because if you do nothing, your joints will become stiff. Having a flare-up is not a reason to avoid activity. In fact, it is necessary to keep moving as well. However, avoid strength training and endurance exercises as you deal with the flare. Instead, try gentle stretches to maintain a range of motion.
Watch What You Eat. While eating is the last thing on your mind during a flare period, eating foods rich in fish and plant oils and avoiding meat can help to reduce inflammation. If you take an omega-3 supplement, increase your intake to 3,000 milligrams daily. Most likely, that consists of taking two omega-3 supplement capsules. However, check the bottle’s label to confirm.
Try Alternative Therapies. As you know, chronic pain and RA patients have found relief in practicing relaxation techniques, mediation, yoga and acupuncture. While I have not tried acupuncture, I have tried and benefited from relaxation, meditation and yoga. All three help during a flare by alleviating stress, relaxing the mind, and relieving pain. When you first try these therapies, becoming relaxed can seem like a nearly impossible task, but it is something that can in fact be learned.
As for acupuncture, researchers have questioned whether it holds any helpful value, but according to many it is a practical alternative for managing arthritis pain. If available during the flare period, it is a viable option that can relieve RA related pain and help to minimize stress and anxiety.
Drug Therapies. When all else fails, it is time to call the big guns. I consider medicinal approaches a last option. RA patients already take plenty of medications to slow down and the stop the progression of the disease, so it makes sense to consider non-medicinal approaches when possible.
Start with over the counter (OTC) anti-inflammatory gels that can be applied to inflamed joints. Use sparingly because overuse of gels can cause skin irritation. If gels are not working, your next option can be anti-inflammatory OTC medications (e.g., Advil or Aleve). Please note that the overuse of anti-inflammatory OTC medications can cause additional risks such as stomach irritation and ulcers so, as with gels, use in moderation.
Call your Doctor. When non-medicinal approaches, exercise and rest, watching diet, alternative therapies, and anti-inflammatory gels and pain relievers are not working, work with your doctor to create a plan that will help you bounce back quickly. Your doctor can raise the dosage of RA medications and prescribe additional medications to help with pain and reduce inflammation. If your flare is especially severe, strong anti-inflammatory corticosteroids can be temporarily used.
Having your own Cheat Sheet
Having rheumatoid arthritis requires you to constantly be on top of your game. This is because a flare-up can keep you out of commission for days on end. As a result, planning for a flare is critical and it is similar to planning for a disaster. Prepare your own cheat sheet even if it is as simple as a post-it note reminder. Keep in mind that planning for flares will help you to cope from the first onset and will allow you to remain capable and focused during a flare period. It will also save you time and energy that is better suited for coping.