Detailed Information About Polymyalgia Rheumatica
Polymyalgia Rheumatica is characterized by pain with functional disability, and stiffness in shoulders and arms, neck, trunk, pelvic girdle and thighs. These manifestations are more pronounce after rest. It usually appears in people over 50 years and is accompanied by marked elevations of acute phase reactants C-reactive protein, which results in higher elevations of the ESR.
The disease is twice as often in women than in men, although this claim is in question. The incidence is higher in whites and is even greater familial incidence. The average age of onset, in most studies, around 70 years, but there are cases compatible with the diagnosis younger than 40 years.
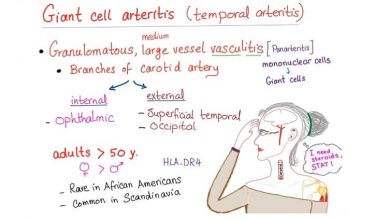
The cause and pathogenesis are not known. The clinical characteristics and the pattern of incidence are similar to giant cell arteritis. The crucial distinguishing feature is the catch in the latter of giant cell arteritis artery biopsy. In fact it is illogical to think that the case of the same disease at different stages concerned or somewhat different expressions of the same process.
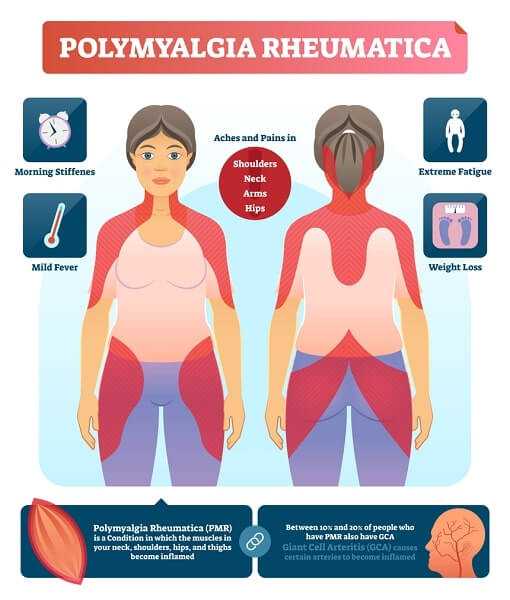
There will be pain, which may be severe, predominantly in the morning and pelvic girdle. The onset is usually insidious with progressive worsening. Rarely the onset is abrupt, but it can happen, once even overnight.
The pain comes with the active mobilization after rest, particularly after resting overnight, although often as it moves and there is pain at rest, even nocturnal pain that prevents sleep. It is accompanied by a sense of rigidity or stiffness. In the early stages the pain usually improves after one or two hours after rising from bed.
The similarity in name, makes the you feel a little confused with the disease fibromyalgia, which has nothing to do with it, because unlike fibromyalgia, polymyalgia rheumatica is an inflammatory disease that causes abnormalities in blood tests and has specific diagnostic tests and treatments.
The most affected tend to settle on their shoulders, followed by the muscles of the neck and gluteal areas and finally the roots of the lower limbs. There isn’t any apparent loss of strength and tendon reflexes are not changed. In some cases it can be seen in the exploration joint pain at the knees and hands in particular. They are also of tendonitis. A diffuse swelling sometimes seen, usually symmetrical, hands or feet. Typically, the coincidence with one or more constitutional symptoms such as fatigue, malaise, weight loss, loss of appetite or fever. In the absence of treatment, the evolution is towards a progressive deterioration and disability.
Laboratory tests are very important. The ESR is a diagnostic criterion and is often a remarkably high as acute phase reactants. The diagnosis was initially uncertain whether it could consider the ESR is less than 40. However, the diagnosis is still supported if the clinic is suggestive and response to steroid treatment in small doses is good, this being a valuable therapeutic trial.
Normochromic anemia is common. Laboratory tests are also essential to rule out potentially clinically similar diseases. It is wise to keep in mind in the differential diagnosis of various diseases as systemic lupus, rheumatoid arthritis, dermatomyositis or polymyositis, paraneoplastic syndrome, leucosis, myeloma and order tests to help us to discard (the study of erythrocytes, leukocytes and platelets, antinuclear antibodies, factor rheumatoid creatine kinase, serum protein, alkaline phosphatase, transaminases, etc). The imaging techniques are less useful, but in any case its usefulness in the diagnosis, differential, since there is no characteristic data or owned by these techniques, in polymyalgia rheumatica.
The pathology is necessary for the diagnosis of giant cell arteritis because this diagnosis is mandatory for the discovery and documentation granulomatous arteritis with features and giant cells in the arterial wall. On the contrary this biopsy pressure, typically of the temporal artery is not considered necessary for the diagnosis of polymyalgia rheumatica. In other words it is not documented inprescindible negative pressure biopsy for diagnosis of polymyalgia rheumatica. Currently, imaging techniques such as intracranial Doppler can help in the diagnosis.
In any case, the rheumatologist may need time to diagnosis in the way of evolution of the disease in each patient and performing tests using cortisone to confirm the diagnosis.
The treatment consists of administering small doses of steroids. If you start with a dose of 10-20 mg of prednisone, the trend has to be, as soon as you find better, the doses will be lowered below 10 mg.
The duration of treatment is impossible to establish. The course of symptoms and laboratory data, especially ESR and C-reactive protein, are the best indicators for monitoring and dose adjustment of steroids and also for the detection of relapses. The evolution of the disease must be counted in months or years and the trend must always be slow and gradual reduction of corticosteroids to their removal. It is possible for polymyalgia rheumatica to gradually improve until all symptoms are gone. An improved diet will help with this process as well.
Polymyalgia Rheumatica Diagnosis
There is no single test for a Polymyalgia Rheumatica Diagnosis for this disease and most importantly to make the diagnosis is the combination of symptoms along with exploration performed by the rheumatologist. The most relevant laboratory test is carried out by raising the Erythrocyte sedimentation rate (ESR), which occurs in the vast majority of patients. The analytical determination is not specific for this condition, and generally elevated in any inflammatory process or infection occurs in the body, but the combination of typical symptoms with the observation of functional limitation and pain in the shoulders and hips, with a marked increase in ESR, attest to the diagnosis if the box occurs in people over 50 years.
The ESR test measures the distance in millimeters from the liquid part of the sanction blood remaining after sedimentation of the cells of the same after spending an hour in a glass column or special tube. In general, the VSG considered normal for men to 15 mm in the first hour to 20 mm in women. In case there polymyalgia rheumatica, these figures reach much higher values, generally above 50 mm.
It is possible that a patient suspected of having Polymyalgia Rheumatica other tests will be performed both analytical and radiological to exclude other processes that may mimic this condition.
Table I summarizes the main signs and symptoms that suggest the Polymyalgia Rheumatia Diagnosis:
Table 1
Common signs and symptoms of polymyalgia rheumatica
In cases of giant cell arteritis or not associated with polymyalgia rheumatic diagnosis, higher doses of corticosteroids are prescribed to control inflation formation of the vascular wall, the order of 40-60 mg. day, although it is possible that lower doses to avoid the risk of blindness, but is not suppressed disease.
The need for treatment varies between 6 months and 2 years on average, may be necessary after declining to adjust the dose if symptoms recur both clinical and laboratory. In some cases where it is not possible to do low doses of steroids because there is insufficient control, you can use other medicines regulators response of the immune response of the individual associated with steroids.
The use of high-dose corticosteroids can cause some side effects, most reversible after discontinuation of therapy, such as fluid retention two, and occurrence of edema and weight gain, enlargement of the face, hair appearance, elevated glucose and osteoporosis in susceptible persons, individually so that the doctor will try to counter these statements with some tips or drugs.
Furthermore, as recovery starts, it is advisable to re-do the kind of active life that existed prior to polymyalgia rheumatic diagnosis and complete with gentle exercises that help to enhance recovery of muscle mass that may have atrophied due to disease, especially in cases of poly-myalgia rheumatica.
Polymyalgia Rheumatica Treatment
This disease is relatively new, known from 1950 so Polymyalgia Rheumatica Treatment is also new. It is seen almost exclusively in people of European origin. The onset begins to appear after 50 years of age and it is also twice as common in women than in men. The main characteristics are muscle pain, especially in the proximal limb regions, such as shoulders, arms, hips and thighs. Its onset is usually acute and there are some patients who can even say the exact day when the problems started.
Frequently have systemic signs such as fever and general commitment to weight loss. The rigidity of the body in the morning, is characteristic. There is an important difference in rheumatoid arthritis is morning stiffness that hands with difficulty using their hands, while in this condition the problem is in the proximal extremities. Therefore it is hard to activities such as getting out of bed, getting up from a chair, getting into a car and even combing. Some patients report difficulty pulling sheets and blankets in the morning. All this with a relatively recent onset.
Despite this tremendous difficulty functioning and pain, the physical examination is negative. No joint inflammatory conditions. You can find some tenderness of the muscles in the proximal limb regions. Usually is not muscular atrophy. Laboratory tests are usually negative, except elevated sedimentation rate is usually over 50. Also found elevated C-reactive protein, sometimes Anemia and impaired liver function tests. It should make specific laboratory tests to rule out other rheumatic diseases.
The diagnosis is made clinically. This is a person over 50 years suddenly began to have pain and stiffness of at least two important areas such as muscles in the region of the shoulders and hips and that takes at least two weeks and the no evidence of infection or other rheumatic condition such as Rheumatoid Arthritis, Lupus or tumor. The diagnosis is confirmed one polymyalgia rheumatic treatment is if this person responds quickly to a moderate dose of corticosteroids.
The cause of this disease is unknown. Very rarely is it associated with temporal arteritis artery. This is an inflammation of the temporal artery, giant cell of undiagnosed can lead to blindness. These patients have pain in the temple area and sometimes you can see the artery that is inflamed. It is associated with headaches and pain in the jaw muscle. It is not known if these two conditions are the same disease at different developmental stages, or if in partnership, both due to a common cause such as inflammation of the arteries in the presence of giant cells.
Treatment of polymyalgia rheumatica is mainly with corticosteroids and is preferably used Medrol or prednisone. Most patients under a doctors care start with 20 mg. per day of prednisone, a single dose in the morning, for a few days and then declined to 15 mg. newspapers and whether this dose the patient reported having improved about 80 to 90% the diagnosis was confirmed. Subsequently the dose of prednisone was gradually decreased in relation to symptoms and the sedimentation rate. Treatment should usually continue for more than one to two years. The anti-inflammatory response is not as good as steroids, and these do not prevent the possibility of vascular complications such as temporal arteritis. They do not serve to confirm the diagnosis, in terms of therapeutic response. Many are known side effects of steroids in high doses (above 10 mg daily) for prolonged periods, such as osteoporosis with vertebral fractures, diabetes, ulcers with and without gastrointestinal bleeding and Waterfalls. That is why the dose should be the lowest possible dose and should be used daily in the morning.
The prognosis of this condition is generally good, provided polymyalgia rheumatica treatment is begins early. The danger lies in not making a diagnosis and develop temporal arteritis that can result in vision loss and sometimes blindness. The other danger is the possibility of side effects of steroids. On the other hand, has recently been shown that polymyalgia rheumatica is associated with cardiovascular disease, which would give a worse prognosis in this disease.
Polymyalgia Rheumatica Tips
If you have been diagnosed with Polymyalgia Rheumatica you may be interested in some tips that will help you in the long run. In the event that this is polymyalgia rheumatica diagnosis, with or without associated arteritis, it is important to follow the polymyaligia rheumatic treatment is generally corticosteroids at established doses. Here are some tips on what to look for and what to look out for:
- Your doctor is the first interested in taking the lowest dose possible but it must be right every time.
- Daily it is recommended to have some muscle toning exercises, especially the extremities. These exercises should not promote any type of strain on the joints but should serve to prevent loss of muscle mass resulting from the stiffness and immobility.
- You must have an appropriate diet to help with your lifestyle. The derivatives of cortisone increases the appetite for something. You should try to maintain your weight. This would be especally helpful if you were in good physical shape prior to coming down with the disease. Your diet must be complete and varied, with intake of foods that are rich in calcium to help compensate for osteoporosis that can be brought on by steroid use.
- If doing well after treatment, but the symptoms reappear, contact your doctor.
- In the event that you only had Polymyalgia Rheumatica and start with a persistent headache, on one or both sides, jaw pain or abnormal vision, you should contact your doctor.
- In case you already were diagnosed with giant cell and you are having treatment and the headache reappeared, please get in contact to your doctor.
Caution should be taken with any polymyalgia rheumatica treatment along with consulting a doctor to ensure proper treatment. Once diagnosed gradually resume your activities and follow instructions so you will not further aggravate your condition. The saying ‘use it or lose it’ is important to keep in mind with polymyalgia rheumatica so the more active you can be with following doctors orders will help you through this.