Discectomy Surgery – What is it?
If you are suffering from radicular pain with numbness, weakness, and a progressive loss of coordination in the limbs then you may need discectomy surgery to remove herniated disc material that is compressing nerves in the spine. These paraesthesias and symptoms such as back pain and neck pain are indicative of spinal nerve compression from bulging and herniated discs which can occur through acute injury and trauma to the spine or chronic wear and tear over time.
Degenerative disc disease is a common condition with almost all people over fifty years old displaying some degree of disc degeneration. Most patients with back pain due to a bulging or herniated disc will be advised to follow a course of conservative treatment for six months or so before back surgery is recommended. In a small number of cases where there is acute risk of paralysis or major loss of motor control, numbness, weakness, and/or severe pain it may be advised to undergo back surgery more promptly in order to relieve nerve pressure and, hopefully, allow the body to begin the healing process so as not to lose function and sensation.
What Happens During Discectomy Surgery?
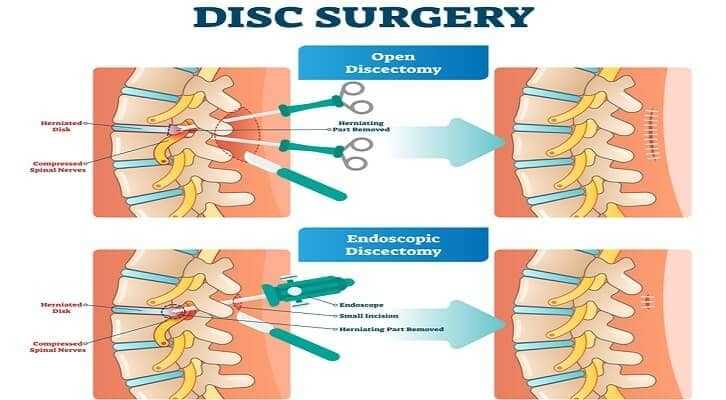
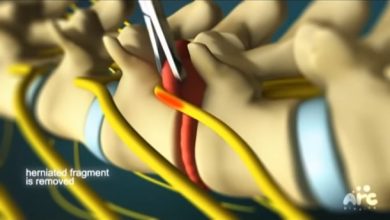
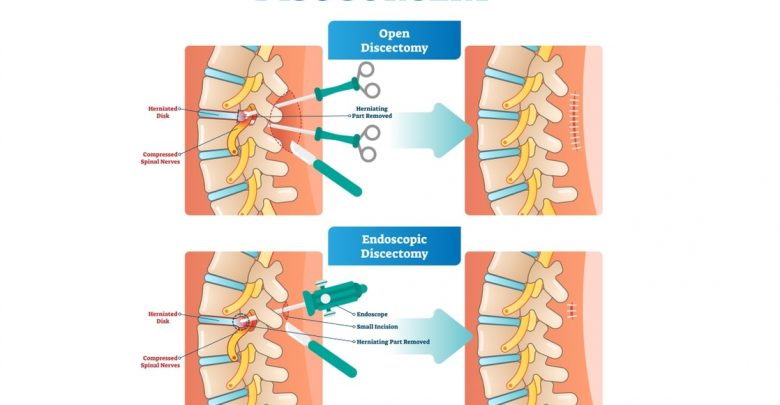
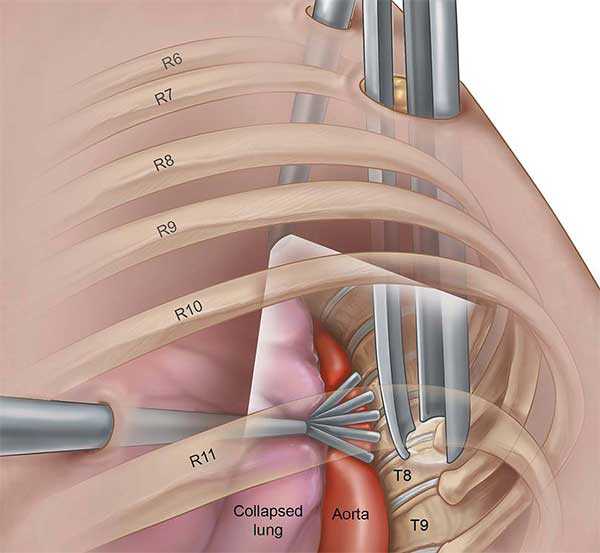
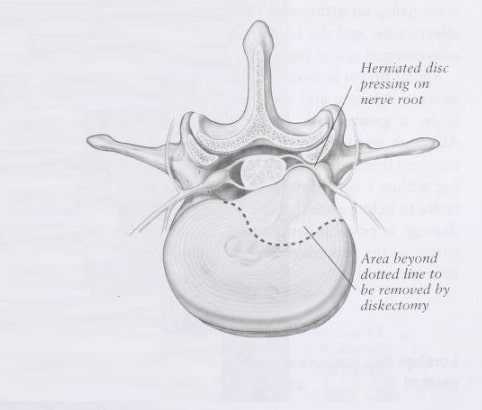
A discectomy is a type of back surgery that involves the removal of the whole or part of one or more of the intervertebral discs in the spine. This may be carried out across a number of spinal levels in which case a traditional open surgical method is likely to be used in order to access a wider expanse of the spine. Spinal fusion will usually follow multiple discectomy surgery so as to maintain the intervertebral height and prevent spinal curvature or spinal slippage (spondylolisthesis). If just one spinal disc is to be removed then the surgeon may make use of minimal access techniques to reduce tissue trauma. A foraminotomy with a discectomy may be performed so as to access the disc space through the foramen and also remove any osteophytes that may be adding to nerve compression in the spinal column.
Minimally Invasive Discectomy Surgery
Minimally invasive surgery such as a microdiscectomy usually takes less time than a traditional open discectomy surgery (around 45 minutes compared to 70 minutes or more). Alternatively, a microlaminoforaminotomy may be conducted in which the surgeon removes a tiny portion of the back bone so as to gain access to the disc and then extract the degenerated disc through this window. Minimal access surgery using endoscopic back surgery techniques can be carried out under local anaesthetic in many cases and removes the need for an extended hospital stay. Recovery periods from a microdiscectomy are also usually shorter than for traditional open back surgery and the degree of nerve trauma, muscle and ligament trauma, and risk from anaesthetic or blood thinning drugs are also lowered.
Where evidence of several damaged discs is present from MRI scans or X-Rays it may be necessary to undergo open discectomy with spinal fusion however, as trying to remove significantly degenerated disc fragments with minimal access increases the risk of leaving material in the area which will continue to irritate and compress nerves. Those with a larger body mass are also less likely to be able to undergo microdiscectomy as there may be difficulty gaining sufficient access to the spine through adipose tissue on the back. An anterior approach may be used for those with a herniated disc in the neck and anterior cervical discectomy with fusion (ACDF) is common in such cases so as to maintain the structure and stability of the cervical spine.
Will a Discectomy Relieve Back Pain?
Patients usually experience considerable relief from neck pain after discectomy surgery, sometimes within a minimally invasive back surgery itself as the pressure is taken off the nerve(s). Where nerve compression has continued unchecked for a significant time however it is likely to take longer to heal such damage and symptoms should gradually dissipate over the weeks and months after surgery. In some cases the extent of damage may prove too much for the body to heal and there will be some degree of residual back or neck pain after discectomy. Those undergoing back surgery are encouraged to quit smoking, maintain adequate hydration and optimum nutrition, carry out good postural practices and, with a physical therapist, devise a regime of stretching and strengthening exercises for a herniated disc. Quitting smoking is particularly important should a discectomy with fusion be necessary as smoking severely compromises spinal fusion success rates. Discectomy surgery can be carried out using both traditional and endoscopic techniques and may help relieve back and neck pain caused by degenerative disc disease.