Drugs Used in the Middle Stage of Alzheimer Dementia

Behavioral problems are the hallmark of this stage of the disease. These include hyperactivity and restlessness, sleep disturbances, resistiveness, and assaultiveness. Many of these problems can be symptomatically managed by modification of the patient’s environment, gentle persuasion, and exercise, but in most cases, sooner or later, the patient requires a psychotropic medication. Initially, drugs with fewer side effects, mainly hypnotics are used, and only if these drugs are not effective, are neuroleptics used. The effectiveness of (β-adrenergic blocking agents, another class of drugs, in the treatment of behavioral problems of Alzheimer patients needs to be further investigated.
Hypnotics
The hypnotics include drugs with mainly hypnotic effect (e.g., diphenhydramine and chloral hydrate) and the benzodiazepines, which in addition to the hypnotic effect also have antianxiety and anticonvulsant effects. The contribution of anxiety to a patient’s restlessness is difficult to determine. In some cases hospitalized patients become more restless after a visit of a family member and appear to be anxious. However, benzodiazepines do not appear to be significantly more effective than diphenhydramine in the treatment of these patients. All drugs from this group, however, are useful for treatment of disturbances of the sleep-wake cycle, which are quite common in this stage of Alzheimer dementia.
Diphenhydramine
Originally developed as an antihistamine, diphenhydramine (Benadryl) has a pronounced sedative effect. It is a common ingredient of nonprescription sleeping pills. In addition to its antihistamine effect, it also has anticholinergic activity. However, with doses used clinically the incidence of anticholinergic side effects is quite low. The maximum activity of diphenhydramine occurs approximately 1 hour after administration and lasts 4 to 6 hours.

Diphenhydramine should be given with caution to patients with a history of bronchial asthma or increased intraocular pressure (glaucoma). Monoamine oxidase inhibitors potentiate the anticholinergic effects of diphenhydramine. The sedative effect of diphenhydramine is not very strong. In a study of elderly women, a 50 mg/70 kg dose of diphenhydramine did not produce significant sedation. However, in Alzheimer patients diphenhydramine is quite effective both as a daytime sedative and as an evening hypnotic in doses of 25 to 50 mg.
Benzodiazepines
All benzodiazepines have hypnotic, antianxiety, and anticonvulsant effects. They are not selective for one or the other effect, although some are marketed as hypnotics (e.g., flurazepam [Dalmane], triazolam [Halcion]), some as antianxiety agents (e.g., lorazepam [Ativan], prazepam [Centrax], chlordiazepoxide [Librium], halaze-pam [Paxipam], clorazepate [Tranxene], alprazolam [Xanax]), and others as anticonvulsants (e.g., clonazepam [Clonopin], diazepam [Valium]). All act by potentiating the effect of the main endogenous inhibitory neurotransmitter, y-aminobutyric acid (GABA). GABA increases permeability of nerve membranes for chloride ions that results in hyperpolarization. Benzodiazepines differ in their time of onset and duration of action.

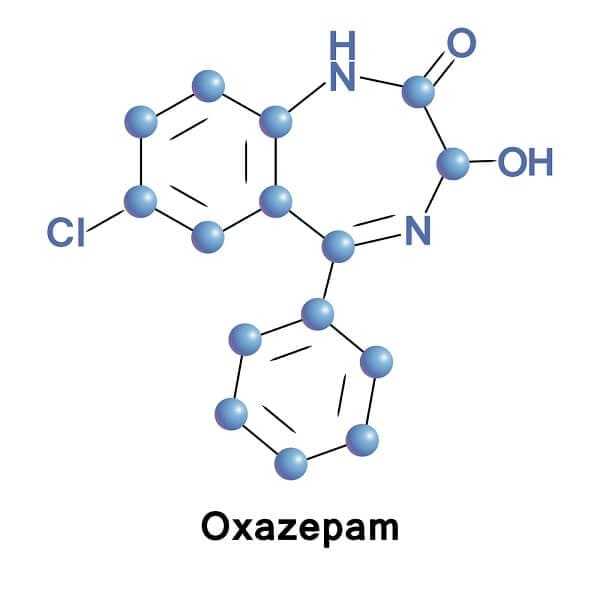
Oxazepam
Oxazepam (Serax) is a short-acting benzodiazepine with a relatively slow onset of action. The maximal effect appears approximately 2 hours after oral administration and is maintained for 8 to 12 hours. Oxazepam is inactivated by conjugation with glucuronic acid in the liver and other tissues. Since this process is not limited to hepatic microsomes, oxazepam is safer than other benzodiazepines in patients with liver disease and in elderly patients. The main disadvantage of oxazepam is the occurrence of paradoxical stimulation in some patients. This stimulation, which is similar to alcoholic intoxication, occurs about 1 hour after oxazepam administration and lasts 30 to 60 minutes. In some patients, oxazepam loses its effectiveness after being used for several weeks. It is not clear if this is due to the progression of the disease or to development of tolerance. Oxazepam, like other benzodiazepines, should be discontinued gradually to prevent a withdrawal state that could precipitate convulsions.
Diazepam
The onset of action of diazepam (Valium) is very rapid and the action is prolonged. Diazepam has a long biological half-life (1 1/2 days) and is metabolized in the liver into an active metabolite that has an even longer biological half-life. Therefore, prolonged diazepam administration can lead to accumulation of diazepam and its metabolite and to a gradual increase in sedation. In elderly patients low doses of diazepam should be used (2 to 5 mg) because its metabolism is decreased with age. Diazepam has strong muscle relaxant activity and it has been found to be useful in some patients who develop muscle rigidity.

Temazepam
Temazepam (Restoril) is marketed as a hypnotic. It has a slow onset of action and its effect lasts about 8 hours. Thus it is useful in patients who have little difficulty falling asleep but tend to wake up during the night. Development of tolerance is a major problem when temazepam is used on a regular basis. Therefore, diphenhydramine is used for initial treatment of sleep disturbances, and temazepam is not used in patients who are receiving other benzodiazepines during the day. In patients who have difficulties falling asleep but sleep well after they do fall asleep, triazolam (Halcion) might be a better choice because of its fast onset of action. However, its therapeutic effect lasts only about 6 hours and a rebound anxiety during the next day has been described.

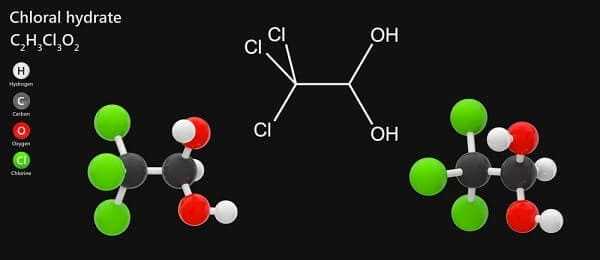
Chloral Hydrate
Chloral hydrate decreases sleep latency and the number of nocturnal awakenings and has very little effect on rapid eye movement (REM) sleep. The mechanism of action of chloral hydrate is not well understood. The hypnotic effect appears to be mediated by its metabolite trichloroethanol, which has a biological half-life of 8 to 10 hours. The adverse effects of chloral hydrate include gastrointestinal irritation and rare allergic reaction. Although its metabolism is not affected by aging of the individual, chloral hydrate does influence the metabolism of several drugs. This effect is mediated by either inhibition of their liver metabolism or by displacement of these drugs from protein binding by one of the chloral hydrate metabolites, trichloracetic acid. Chloral hydrate should not be given to patients with significant liver or kidney impairment. It is useful in patients receiving benzodiazepines during the day whose sleeping disturbances do not respond to diphenhydramine.
β-Adrenergic Receptor Antagonists
β-Adrenergic receptors are present in the heart, blood vessels, bronchial and other smooth muscle, fat tissue, brain, and other organs. There are two types of β-adrenergic receptors: β1, located in the heart, and β2, located in smooth muscles. β-Adrenergic receptors mediate stimulation of heart rate and contractility, vasodilation, bronchodilatation, and some metabolic processes. β-Adrenergic receptor antagonists are used mainly in the treatment of cardiovascular diseases, including hypertension, coronary artery disease, cardiac arrhythmias, and migraine headache. However, they also have some effects on the brain and have been found to prevent anxiety states (stage fright) and to produce depression as a side effect when used for the treatment of cardiovascular diseases.
Several β-adrenergic receptor antagonists are available for clinical use. The oldest drug in common use is propranolol (Inderal), which blocks both types of β-adrenergic receptors. Other β-blockers (e.g., metoprolol [Lopressor]) are selective for β1-receptors or block β-receptors only partially (e.g., pindolol [Visken]). Propranolol has been reported to decrease the occurrence of rage and violent behavior in patients with brain damage due to a trauma, infection, alcohol abuse, or anoxia. The same effect has been reported for pindolol, which has the added advantage that it does not decrease the heart rate as much as propranolol and, therefore, it does not have to be discontinued because of bradycardia.

Evidence for the effectiveness of β-adrenergic blocking agents in treatment of Alzheimer dementia is much weaker. Petrie and Ban described three patients with the clinical diagnosis of Alzheimer dementia whose agitation was improved by propranolol treatment. A decrease in patients’ pacing behavior after propranolol administration has also been observed, but often the pacing was replaced by a bizarre behavior (e.g., rearranging of furniture, removing railing) that was more disruptive than pacing.
β-Adrenergic blocking agents should not be administered to patients suffering from bronchial asthma because they could precipitate an asthmatic attack. In this respect selective β1-blockers are safer than nonselective ones. β-Blockers also should not be administered to patients with sinus bradycardia and cardiac block or to patients with marginal cardiac function because they could precipitate congestive heart failure. β-Blockers should be given with caution to patients with diabetes mellitus, because they block tachycardia induced by hypoglycemia, and to patients with hyperthyroidism, because they mask some symptoms of this disease. The dosage of β-blockers should be decreased gradually to prevent rebound coronary ischemia and hyperthyroidism.
Neuroleptics
Despite the effectiveness of drugs mentioned in the previous sections, most Alzheimer patients sooner or later require treatment with neuroleptics, which are more effective for treatment of behavioral problems than benzodiazepines.
These drugs were developed for the treatment of psychotic disorders. The antipsychotic effect is presumably generated by the blockade of dopaminergic receptors in the brain. It is not clear if this is also the mechanism of their action in Alzheimer patients. Although “psychotic symptoms” (e.g., hallucinations and delusions) occur in some Alzheimer patients, they are relatively uncommon and may not be directly related to behavioral problems seen in most Alzheimer patients. In addition to the effect on dopaminergic receptors, neuroleptics also affect a-adrenergic, histamine, and serotonin receptors. It is possible, therefore, that the beneficial effect of neuroleptics in Alzheimer dementia has a different mechanism of action than the antipsychotic effect.
Unfortunately, all neuroleptics often produce undesirable effects. The most common of these are extrapyramidal effects, anticholinergic effects, and postural hypotension. The most common extrapyramidal effects are muscle rigidity and tremor at rest. Other extrapyramidal effects include acute dystonia (spasm of muscles of tongue, face, neck, or back) and akathisia (motor restlessness), which may occur soon after initiation of neuroleptic therapy, and tardive dyskinesia (involuntary movements of face and other muscles), which may occur when neuroleptics are used chronically. Anticholinergic effects include dry mouth, blurred vision, constipation, and urinary retention.

According to the incidence of undesirable effects, it is possible to distinguish two groups of neuroleptics. Drugs from one group (e.g., haloperidol [Haldol], thiothixene [Navane]) produce more extrapyramidal effects but have little anticholinergic activity. Drugs from the second group (e.g., chlorpromazine [Thorazine], fluphenazine [Prolixin, Permitil]) produce more anticholinergic side effects but less extrapyramidal effects. Both of these groups seem to be equally effective in treatment of behavioral problems in Alzheimer patients. Therefore, the choice of an agent depends on the patient’s condition and the probability and danger of these two kinds of undesirable effects. It is more important to avoid anticholinergic effects in a patient with prostatic hypertrophy, or who still has some preserved memory function, than in a patient who is in a more advanced stage of dementia and has some signs of muscle rigidity.
In addition to the three main adverse effects described above, neuroleptics may also produce sedation. Hypersensitivity to neuroleptics may also occur and lead to rash, dermatitis, or jaundice. To prevent neuroleptic side effects it is important to use the lowest effective dose and to reevaluate the need for treatment periodically. Very commonly with progression of Alzheimer dementia, the need for neuroleptic medication decreases and only a few patients in the late and terminal stages of Alzheimer’s disease require neuroleptic medication.
Haloperidol
The main advantage of haloperidol (Haldol) is the lack of anticholinergic activity. Haloperidol is effective in low doses (0.5 to 1 mg twice or three times a day) in controlling behavioral problems of Alzheimer patients. However, the incidence of extrapyramidal effects is rather high. A cholinergic receptor antagonist (e.g., benztropine [Cogentin], trihexyphenidyl [Artane]) has sometimes been added to haloperidol treatment to prevent or to decrease extrapyramidal effects. However, this approach negates the advantage of haloperidol over neuroleptics with anticholinergic activity. If extrapyramidal effects pose a problem, it may be better to switch from haloperidol to another neuroleptic with lower incidence of extrapyramidal effects.
Thioridazine
Thioridazine (Mellaril) is another neuroleptic that has been consistently found to be effective in the treatment of behavioral problems in Alzheimer patients. It is metabolized into an active metabolite mesoridazine (Serentil), which is itself also used as a neuroleptic. Thioridazine produces fewer extrapyramidal symptoms than haloperidol but is more likely to cause anticholinergic effects and postural hypotension. Low doses are again effective, ranging from 10 mg twice a day to 25 mg three times a day.
Loxapine
Loxapine (Loxitane) is a neuroleptic that has been found to be as effective as thioridazine in the treatment of behavioral problems in Alzheimer patients. The incidence of orthostatic hypotension in patients treated with loxapine is lower than in patients treated with thioridazine. The dose of loxapine is 2.5 to 5 mg twice or three times daily.