Facet Joint Treatment Options
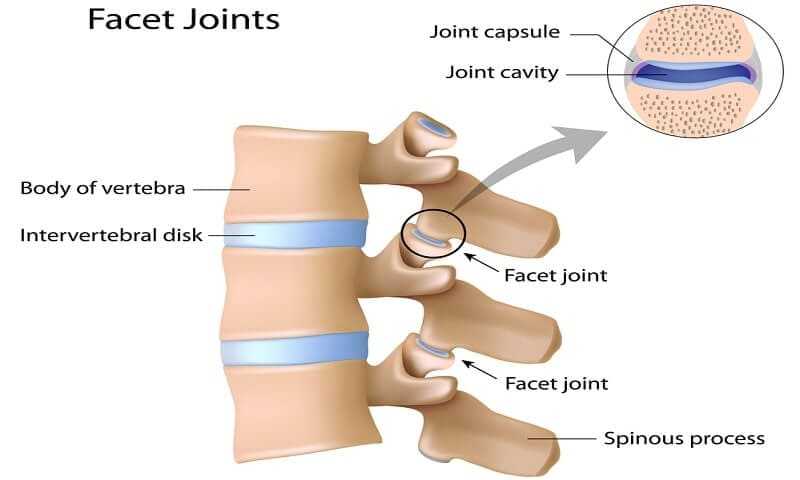
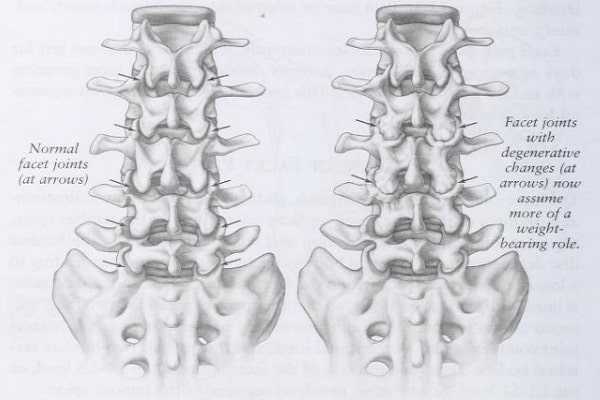
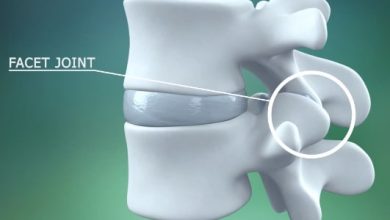
The facet joints, also known as the zygapophysial joint, are synovial joints in the back of the spine that are contained within a fibrous capsule. These joints are found on either side of the spine where the inferior articular process meets the superior articular process at each side of the vertebrae. Facet joints allow movement in the spine and are, therefore, subject to considerable wear and tear over the years. Although the facet joints themselves do not contain free nerve endings, they are innervated by mechanoreceptors. Whiplash, and contact sports injuries can stretch the synovial capsule and cause prolonged nerve problems leading to muscle cramps and tenderness in the back. Facet joint problems may also contribute to other structural defects in the spine and are in themselves often a result of other spinal pathology.
Facet Disease Symptoms
Symptoms of facet joint disease are usually localized to the area around the joint itself, with tenderness, and an aching, uncomfortable feeling in the back that may move, or radiate to other area of the back, shoulder, or hip. Pain-maps can help identify the root of the pain Dwyer (1990), but diagnostic imaging often clouds the issue as many patients have additional spinal stenosis, spondylosis, and other degenerative spinal issues both with and without neck pain. Facet joint problems frequently coexist with disc herniation or degenerative disc disease, ligament calcification, and muscle or nerve problems. Manchikanti (2004) found that the facet joints were implicated as a cause of chronic neck pain in 54-67% of patients, 15-45% of patients with low back pain, and 48% of patients with thoracic pain. Some patients experience acute, unpredictable, episodes of acute facet joint pain a few times a month or year. Other symptoms include pain on extension or rotation of the neck, numbness and muscle weakness, headaches and neck pain, and a dull, aching.
Conservative Treatment for Facet Disease
Back surgery is usually the last recourse for treating back or neck pain, with patients encouraged to try at least six months of conservative treatment prior to considering surgical intervention. Physical therapy alongside analgesic and anti-inflammatory medications can effectively relieve back pain, with ice packs helpful to treat inflammation, oedema and muscle spasm. Many patients have selective nerve root blocks as part of the diagnostic procedure for facet joint syndrome and these frequently provide a degree of pain relief, although often fairly short-lived. However, medial branch blocks may, unfortunately, have adverse effects on balance and lead to presyncope being experienced by some patients (Barnsley, 1993).
Cognitive behavioural therapy may be indicated in some cases, as patients can become anxious about restrictions in activity and exacerbate the degeneration through a sedentary lifestyle. Patients are sometimes told that the condition is ‘all in their head’, which rarely leads to an effective relationship between them and their doctor. Thorough diagnosis, involving a detailed symptom history, and a trial and error approach to pain management is effective in most cases, with back surgery for facet joint disease postponed as long as possible for the majority of patients.

Facet Disease Surgery
Back surgery for facet joint disease and back pain may involve facetectomy (either whole or partial), cervical spinal fusion, or foraminotomy, largely depending on the severity of the condition and the presence of other structural pathology. On occasion as surgeon may be able to reduce facet joint pain by simply removing some of the osteophyte growth seen with this condition. However, the body creates these bone spurs in an effort to stabilize the spine so they may simply grow back or other problems of spinal instability may arise. A foraminotomy where the exit space for spinal nerve roots is increased can address part of the problem for many patients, as can the removal of herniated disc fragments causing nerve and spinal cord compression. Ligament calcification may also be causing problems with the facet joints’ mobility and these may be severed or removed to aid flexibility.
When a simple facetectomy is performed, patients are usually mobile after a day or two, with some physical restrictions for several weeks on activities that can jolt or stress the spine (heavy lifting, twisting, bending, and running, for example). More minimally invasive procedures, such as laser spine surgery are being developed for facet joint disease and usually have significantly lower risks and a shorter recovery period. Laser spine surgery is limited however in terms of how much material can be removed from the spine, and an open procedure is still indicated when the entire facet joint is to be removed.
Another surgical option is the use of percutaneous radiofrequency neurotomy. This procedure denervates the facet joint through coagulation of the medial branch of the dorsal ramus. The nerve is not destroyed because the medial branch cell bodies remain intact in the dorsal root ganglion. The procedure does prevent the pain signals transmitting along the nerve to the dorsal root ganglion until the nerve grows back within 6-9 months (in most cases). At this point the neurotomy can be repeated as it is an effective method of pain relief in most (c70%) sufferers of whiplash-induced cervical facet joint disease. This minimally invasive procedure may also be referred to as facet thermal ablation and multiple procedures can provide effect treatment for many years without the need for more invasive surgery.