Faq about Heel Pain
What causes heel pain?
Heel pain is caused by many different conditions. There are a number of structures that attach on the heel or work through and around the heel. Each of these structures in some way can cause heel pain. The most common cause of heel pain is due to inflammation and strain of a ligament called the plantar fascia. This causes far and away the most number of cases of pain under the heel and arch. This condition is often erroneously blamed on a heel spur, as a spur may or may not be actually present but rarely ever actually causes pain itself. Other causes of pain to the bottom of the heel include nerve inflammation, a bruise (often called a stone bruise), inflammation of a bursal sac, a heel bone stress fracture, bone cyst, and symptoms related to body-wide arthritis. Pain on the back of the heel is still very common, although not as common as pain on the bottom of the heel. It is usually caused by inflammation of and damage to the Achilles tendon, as well as irritation from a bone spur or calcification on the back of the heel bone. Each of these conditions is discussed in more detail on this website.
Do flip flops cause heel pain?
Flip flop sandals are commonly worn in the summer, and often year round in warmer climates. These sandals have varying degrees of construction quality, but most fit into a category of inexpensive and poorly supportive footwear. Most flip flops, especially those found in discount department stores, resort boutiques, and many discount shoe retailers are simply rubber or foam soles with a strap to help the toes keep the sandal on. In general, these sandals have no structural support, and the foot functions essentially as it wound barefoot. The sole of the sandal offers protection from sharp objects, without offering any other function. The strap required to keep the shoe on actually causes more strain to the foot as the effort to keep the sandal from slipping by gripping the the toes forces the foot to use muscles abnormally.
Flip flop sandals can contribute to heel pain in the same way that barefoot walking causes strain to the plantar fascia. Because the sandal provides little to no support, the arch becomes just as strained as would be seen with barefoot walking, perhaps even more so because of the gripping motion needed to keep the sandal on. What results is a greater tendency towards plantar fasciitis than with the use of a standard shoe.
Some flip flop sandals are designed better, and do have increased arch support with better quality materials in the sole. There are several brands on the market designed for just such a purpose. Our doctors can discuss these sandals with you, as new products are introduced every year to the market.
Does heel pain need to be treated with surgery?
Surgery may be necessary in some cases of heel pain, but the majority of cases do not require surgery to relieve the pain and keep it away.
Most cases of pain in the bottom of the heel, usually caused by inflammation to the plantar fascia, respond well to treatment that reduces the inflammation and reduces the mechanical forces that cause the injury in the first place. Surgery is usually performed less than 5% of the time in these cases.

Case in which there is pain to the back of the heel are a little different, as the bone on the back of the heel is often involved in the condition. Because of this, surgery is needed more often to reduce the irritating bone and repair the damaged tendon often the source of the pain.
Can the plantar fascia be torn?
The plantar fascia is a ligament on the bottom of the foot. While it is strong and thick, it is prone to weakness and injury. Sometimes, the injury can be so strong that the plantar fascia ruptures, essentially tearing across part of its width. This tear causes immediate and significant heel and arch pain, and may take a couple months to recover from.
There are also times in which the plantar fascia can gradually weaken due to arch strain and inflammation, and spontaneously rupture without significant injury. This is not as common as a traumatic rupture, but can be just as painful.
Plantar fascia ruptures require some form of immobilization to allow the ruptured tissue to heal. This process can take 1-2 months, and often involves the use of a walking boot.
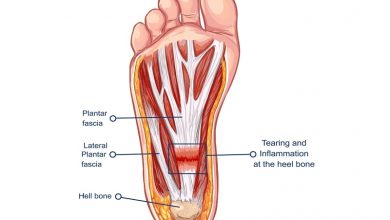
What is the plantar fascia?
The plantar fascia is a thick fibrous band of tissue that forms from the bottom of the heel bone to the bones in the ball of the foot. It is a firm, rubbery strap of tissue that is technically a ligament, since it connects several bones together. There are three sections to this fascia- the medial band runs closer to the inner side of the foot, the intermediate band is located centrally, and the lateral band is located closer to the outer side of the foot.
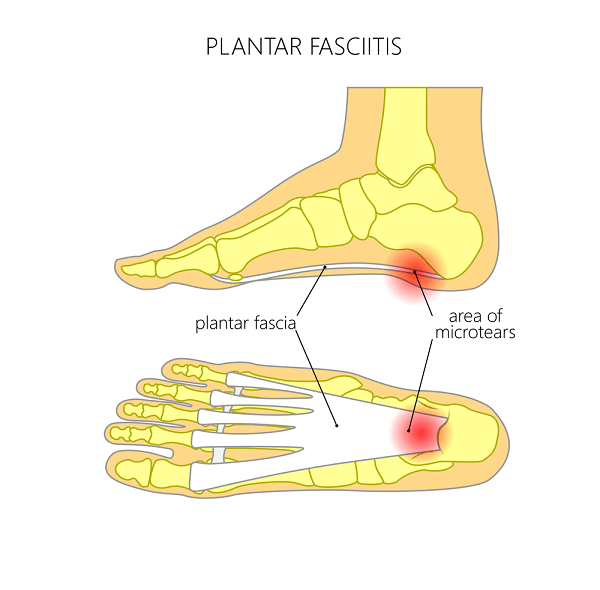
The plantar fascia stretches as one walks or stands, and it has to remain somewhat flexible. Because of this stretching, the plantar fascia is at risk for tissue injury, especially in people with flat feet. The inflammatory condition that follows is called plantar fasciitis, and it is the top cause of heel pain.
Plantar Fasciitis FAQs and Answers
Why does the back of my heel hurt?
Pain on the back of the heel is caused by either injury and inflammation of the Achilles tendon, a bone spur on the back of the heel, or a combination of both. The Achilles tendon is very strong, but it can degenerate and weaken, leading to inflammation and pain. This degeneration can also be caused because of tendon irritation by a bone spur located behind the tendon off of the heel bone. At other times, an abnormal enlargement of the heel bone can cause pain as it rubs against one’s shoe, without directly irritating the Achilles tendon.
If the Achilles tendon continues to degenerate, it can potentially rupture, which is a very serious injury that requires surgery.
Pain on the back of the heel should be treated promptly, as it can last for many years if allowed to continue untreated.
Can Gout Cause Heel Pain?
Gout is a condition that involves an abnormal level of the crystal-based chemical uric acid, a by-product of the digestion of certain foods. This crystal builds up in the blood stream, and then deposits into joints, commonly in either the big toe joint or the ankle. Symptoms often include a red, hot, swollen joint with extreme pain to even the touch of a bed sheet.
The heel, either on the bottom or the back, contains no joint structure for the uric acid to deposit into. For this reason, gout is not a primary cause of heel pain. However, if gout is present in a nearby joint, like the ankle joint, the inflammation from this condition can aggravate the heel tissue, and pain can be felt in the heel indirectly due to gout itself.
Is heel surgery required to treat plantar fasciitis?
Plantar fasciitis is a heel pain condition that usually responds well to non-surgical treatment. Because it is often a disease related directly to one’s foot structure, conservative treatment works well to cure the condition. This is accomplished by reducing the painful inflammation through medication and therapy as well as controlling the forces that cause strain to the plantar fascia with more stable shoes and proper shoe inserts. Less than 5-10% of patients with plantar fasciitis need aggressive measures like surgery to relieve plantar fasciitis.
That being said, a small number of people with plantar fasciitis do not get better with multiple measures over several months, and require heel surgery to get them full relief.
How do I know if I have torn my plantar fascia?
Plantar fascia tears are not nearly as common a source of heel pain as plantar fasciitis, in which there are only microscopic tears. The plantar fascia can tear from either a violent force on the bottom of the foot forcing the front part of the foot upward, or from a more gentle force acting on a weaken fascia that has become degenerative from chronic fasciitis.
Regardless of the cause, the symptoms of a plantar fascia tear include a sudden, sharp, searing pain in the arch, and often includes the sensation of a pop or snap. Externally, swelling and bruising can be see. The bottom of the arch will be very painful to bear weight on, and a sense of foot weakness may also be present.
The plantar fascia actually has three bands, and it is very uncommon for all the bands to rupture together. More typically, one or two bands will rupture rather than all three. Because of this, the foot does not structurally change much during a fascia rupture. The foot does not usually look flatter.
A plantar fascia rupture is treated a little differently that plantar fasciitis, as the torn tissue needs to mend with more support during the healing process than it does when the condition is simply fasciitis.
Can heel pads help with pain on the bottom of the heel?
It is often assumed that heel pads can cushion the bottom of the heel and help reduce pain. Many people go to the pharmacy for this very reason when heel pain initially develops, and purchase heel pads. Unfortunately, these products do not work for most cases of heel pain.
The cause of pain under the heel most of the time is plantar fasciitis, which is inflammation of a ligament found in the arch. The inflammation is usually at where this fascia attaches to the heel, but simply padding the heel will not reduce the underlying arch strain which is the cause of the inflammation in most cases. What is needed actually is an arch support. By reducing the arch strain, the plantar fascia is better supported and the inflammation can be reduced when other treatment methods are used to reduce the overall inflammation in the heel. Heel pads do not generally help with this condition. Unfortunately, there are only a few brands of over-the-counter arch supports that are of sufficient quality, as most are too soft and compressible and some, such as those found in retail arch support stores, are far too hard as a general all-purpose insert. Many people with this condition rely on prescription orthotic inserts for long term arch support. However, most do well to at least start with a quality over-the-counter support.
Heel pads can be of benefit for one specific less common cause of heel pain, which is bursitis. In this case, there is inflammation to a pad of tissue directly under the heel bone, and heel padding, particularly gel pads, can reduce the shock to this area. Heel bursitis can be present at the same time as plantar fasciitis, but most quality arch supports include some form of heel padding, including Powerstep inserts.
How does heel pain differ in adults and kids?
There is a significant difference in the reason why kids get heel pain compared to adults. The usual cause of heel pain in an adult is plantar fasciitis, which is injury in a tissue called the plantar fascia,. This is a ligament-like band of tissue on the bottom of the arch. Other conditions can also cause heel pain, as this website discusses in detail. In kids, these conditions typically do not appear until later teen years. When kids get heel pain, the cause is typically due to inflammation in a part of the heel bone called the growth plate. During growth, a child’s bones have areas called growth plates that help grow bone. The growth plate in the heel bone can become inflamed, causing pain to the bottom of the heel during running and jumping. Unlike plantar fasciitis, heel pain in kids cannot be resolved with aggressive medical treatment. This type of heel pain simply takes time to resolve on its own. However, the doctors can help hasten the recovery so the child can return to sports and other activities quicker.
Why does my heel hurt in bed?
Heel pain typically is most active when one is walking or standing, or for a brief period after one has retired to bed, but some conditions can cause pain in the heel to occur for much of the night. These conditions are mainly related to nerve damage, unlike plantar fascia or tendon damage that causes most cases of heel pain. The most common cause of bedtime heel pain is compression on the nerve in the lower spine, which is worsened when one is lying down or seated. The pain often is felt as a broad burning or pins and needles tingling sensation, and is usually felt in one heel rather than both. It can be accompanied by thigh or hip burning as well as some shooting pain in the leg. There is little to no pain felt when one is walking or standing. Another cause of nerve-related heel pain is peripheral neuropathy, which is nerve disease due to an underlying medical condition. Many conditions can cause these symptoms, including diabetes (the most common cause), as well as thyroid disease, vitamin B and folate deficiencies, prior alcoholism, and some infections. This condition can also have no specific cause, and is seen in older age groups. The pain is often felt in both heels at random times although it is seen more frequently at night, and can be associated with symptoms going up the leg to the knee.
Why does my heel pain hurt worse in the morning or after I get up after sitting?
The most common cause of heel pain, plantar fasciitis, is often (but not always) more painful in the morning or after getting up from rest in a chair or other seated position. This is due to the fact that the plantar fascia receives the most amount of strain after it has had a chance to tighten up. This occurs when one if off their feet for a short while, as the lack of bearing weight does not allow for the fascia to stay more limber. As one get up from rest, the fascia stretches again, and in some cases can tear microscopically, leading to more immediate pain. The pain eventually reduces with more activity, at least temporarily.
Not everyone with plantar fasciitis has this pain after arising, although most people do feel greater pain the longer they are active on their feet. This is due to the fact that continued strain to the fascia, while initially stretching the tissue, eventually surpasses the tissue’s tolerance for strain, and painful inflammation develops. This process becomes a never ending cycle for most people with plantar fasciitis, until the cycle is broken by proper treatment of the heel pain.
Why Do My Feet Hurt In The Morning?
How does stretching help with heel pain?
Stretching is a very important part of the treatment for heel pain, and is used in the treatment of several different causes of pain in the heel.

For pain on the bottom of the heel and arch due to plantar fasciitis, stretching is used to keep the plantar fascia limber. When it is better stretched, the fascia has less likelihood of becoming strained as easily after arising from bed or simply walking, leading to less inflammation and therefore less pain.

For pain on the back of the heel, stretching helps keep the Achilles tendon more limber, allowing it to function better and reduce the strain and microscopic tearing the tendon undergoes when it is inflamed. This leads to less pain, and reduces overall inflammation.
Foot stretching exercises for Plantar Fasciitis
When is surgery recommended to relieve my heel pain?
Surgery is used to treat heel pain, but in many cases surgery is delayed until multiple other reasonable treatment methods have been tried. This is especially true for plantar fasciitis, as non-surgical treatment methods are usually successful in ending heel pain. For conditions like Achilles tendonitis with a spur, and tarsal tunnel syndrome, surgery has to be considered earlier as these cases do not always respond to non-surgical treatment.
Your foot doctor will analyze how you respond to your treatment at each visit, and alter the treatment plan as needed to improve your results if you are not healing as expected. At some point, your foot doctor may suggest surgery if you are not improving well enough, or if your pain continues to return after initially resolving.
Please keep in mind that heel pain does not improve instantly with treatment, and some cases may take several months or longer to resolve. Treatment can consist of a variety of therapies, including medication, structural support, physical therapy, and immobilization. When these fail to bring about full relief, surgery is recommended.
Can arthritis cause heel pain?
Heel pain involves parts of the foot that do not have a direct association with a joint. Arthritis is defined as inflammation of a joint and its tissue. The main cause of pain on the bottom of the heel is not related to a joint, and therefore arthritis does not cause or contribute much to heel pain on the bottom of the foot. An exception to this is the effect of rheumatoid arthritis on the foot. Rheumatoid arthritis, as well as other similar types of inflammatory conditions, is a disease caused by an abnormal immune reaction to joint tissue. This condition can lead to inflammation in the tissues on the bottom of the the heel, and can therefore cause heel pain as a secondary effect. However, this is a far different process than traditional arthritis that most people refer to when they speak of arthritis, and its contribution to heel pain is uncommon.
The same can be said about pain in the back of the heel. This location is closer to a joint, specifically the back of the ankle joint. Sometimes spurs along the back of the ankle joint can limit motion and cause pain that refers to the back of the heel. However, this is uncommon and the majority of pain in the back of the heel is related to problems with the Achilles tendon and the heel bone, not a joint or arthritis.
How long does it take to recover from heel surgery?
Heel surgery recovery can vary depending on what part of the heel needs to be operated on, as well as the individual surgery performed.
When the plantar fascia is operated on, the average recovery period is typically about six weeks before one can walk comfortably in shoes. This can vary from person to person, as some people recover faster and others slower. The fascia needs time to heal from the procedure itself, as does the incision on the side of the heel.
Surgery to the back of the heel usually requires considerable more healing time as it often requires removal of the Achilles tendon off the back of the heel bone to access the spurring underneath. The tendon is then reattached, and healing takes place over the course of a month. It takes one to two more months before the tendon attachment is strong enough to withstand daily activity. If the Achilles tendon does not need to be removed, and only the tendon itself needs to be treated, the recovery is typically four to six weeks.
What should I wear around the house to prevent heel pain?
Wearing supportive shoes while walking and standing at home is very important in the treatment and prevention of heel pain. Most cases of heel pain on the bottom of the foot are due to strain under the arch. The flooring at home is no better for this strain than concrete or store tile, even carpet does not offer any substantial arch cushioning. Many people make the mistake of walking barefoot at home when dealing with heel pain, being lulled into the though that their carpets help. This is simply not true.
One needs to wear a supportive shoe at home in the very least, and preferably one needs to wear an arch support insert such as Powersteps or a prescription orthotic. Certainly most regular lace up shoes worn outside can serve this purpose and accommodate an insert. However, many traditional house shoes and slippers are too shallow to be of much support or hold an insert. Many people also understandably do not want to wear their potentially soiled regular shoes indoors.