Deep brain stimulation
Deep brain stimulation (DBS) is an option for patients who have taken standard medications for a number of years, but the drugs are either not lasting long enough or the patient has started to experience side effects. Some people assume DBS is a treatment of ‘last resort’, but Melbourne neurosurgeon Richard Bittar says that’s not the case: ‘It’s offered by doctors when all other reasonable options have been tried, and have either failed or not been tolerated very well.’
This treatment can reduce the severity and duration of motor fluctuations. Sydney neurologist Dr Victor Fung says DBS is not better than medications when they’re working at their peak, with two exceptions.
- It can relieve tremor that is resistant to medication.
- It can reduce dyskinesias (involuntary movements).
The medication (levodopa) was working erratically after a while. The drug benefits begin to wear out Everyone said I was bad. … so I decided to take the plunge.
Peter McWilliam, on his decision to have deep brain stimulation
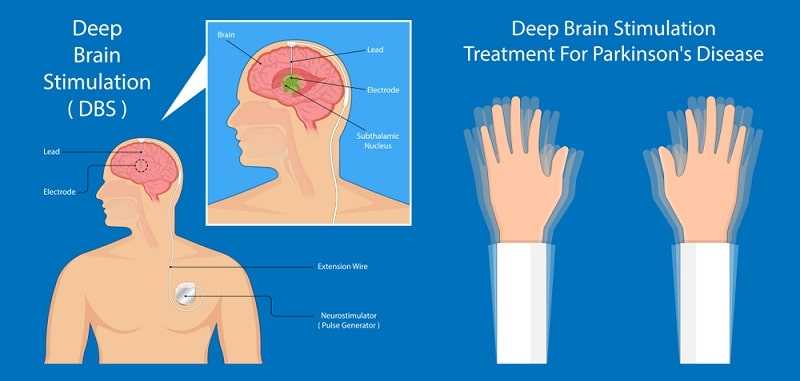
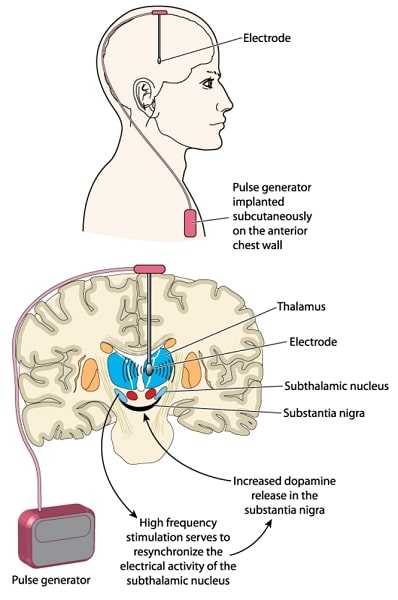
DBS is a surgical procedure that involves implanting an electrode or thin wire through the top of the skull into the area of the brain that causes the Parkinson’s symptoms. The electrode is connected to an extension wire that is placed under the skin of the head, neck and shoulder, and a device similar to a cardiac pacemaker is implanted in the chest or stomach.
The device delivers electrical impulses to the leads that go into the brain. These impulses interfere with and block the abnormal nerve signals that cause the symptoms of Parkinson’s disease.
Before the procedure, the patient has an MRI (magnetic resonance imaging) or GT scan (computed tomography) to locate the area in the brain where electrical nerve signals generate the Parkinson’s symptoms.
The surgery is usually conducted under local rather than general anaesthesia because it’s important for the patient to provide feedback when the doctor is finding the right spot to place the electrode. ‘If we turn the electric charge on and their tremor stops then we know we’re in a pretty good area,’ says Dr Bittar. ‘We also like to see whether they’re getting any side effects. There is no point in fixing someone’s tremor when they’re getting a severe side effect.’

Some surgeons don’t believe that is the case and will perform the procedure while the patient is asleep. But Dr Bittar says, ‘The downside of keeping the patient awake is well and truly justified by the potential benefit—the degree of confidence in placing the electrode and giving the patients the best possible chance of a good outcome.’
Patient Peter McWilliam had some fears about remaining awake on the operating table for several hours while doctors probed his brain. ‘They gave me a sedative drug that made me forget everything that happened on the table. It was less traumatic than going to the dentist,’ he says.
According to Dr Bittar, there is a bit of pain involved. ‘We generally try to use more local anaesthetic and sedation to try and keep the patient as comfortable as possible. It’s not a procedure without discomfort but that’s the price patients pay to increase their chances of getting a good result,’ he says.
Dr Bittar has used DBS for more than 150 patients. He says the surgery has become more popular, since its mainstream acceptance several years ago. ‘That’s partly due to the patients being more aware of its existence and the neurologists being more aware of the potential benefits.’
One in four or five of my patients will come off medication. On average, they reduce their medications by 30 to 70 percent.
Dr Richard Bittar
Deep brain stimulation is a costly operation and not everyone can pay for the treatment.
Even with private health insuranee, Peter MeWilliam was left about $12,000 out of pocket but he says the results are worth it.
What are the benefits?
The beauty of having the surgery is that many patients who experience bad tremor will get a significant benefit. The amount of time patients spend in an ‘off’ state, when they are largely frozen, also improves. Generally, doctors say patients will get the same benefit as when they’re at their peak on medications, except the dosages have been greatly redueed.
Unfortunately, this also means that if the patient is not benefiting significantly from medication, then they may not benefit from surgery (with the possible exception of tremor management). Surgery is also not appropriate for people with significant thinking and behavioural problems. An age limitation also exists. A review by a neurologist experieneed with DBS may be neeessary to decide whether surgery would be appropriate.
Another benefit is that DBS does not damage healthy brain tissue and the procedure ean be reversed if a cure or more promising treatments are found in the future.
The stimulation from the electrodes can also be reprogrammed if the patient’s condition changes, without the need for more surgery. The patient ean adjust the voltage—within a safe range that is chosen by the neurologist. However, any major adjustments are left to the neurologist.
Peter McWilliam says the treatment has changed his life. He describes his life of being a virtual recluse before having the surgery. ‘Before I couldn’t go to a restaurant because I’d put food all over the place. You’re effeetively eliminated from life. Now my physical movements have calmed right down. I can socialise again.’
The surgery has also enabled him to have a good night’s sleep without shaking as hard, and he has had his driver’s license returned, giving him much more independence.
What are the risks?
As with all major operations, the patient faces the risk of infection and complieations. The risk of infection with DBS is about 3 per cent. There is also a risk of major bleeding, which occurs in 2-3 per cent of cases.
Doctors also say there is a one in 100 chance that a patient will die as a result of the surgery. This would generally occur as a result of a massive haemorrhage or stroke. ‘The risks of brain surgery are mildly to moderately increased when compared to most other types of surgery,’ says Dr Riehard Bittar.
Those risks are higher in the elderly, or in patients who have other underlying medical conditions.
Complications from surgery may include cognitive and visual impairment, swallowing difficulty, seizures and headache. Cognitive problems ean occur if there is stimulation of the subthalamic nucleus (STN), a part of the brain which is a popular target for DBS in Parkinson’s patients. The risk of this happening is much greater in patients with cognitive problems before surgery, which is why they are assessed by a neuro-psychologist beforehand to see whether the target needs to be changed. Dr Bittar says that ‘swallowing problems, seizures and visual impairment affects less than 1 per cent of patients as a result of the surgery. Headaches can occur for a few weeks after having the procedure, usually because of air inside the skull. Headaches generally settle completely.’
Who can benefit from DBS?
The benefits of DBS surgery mirror the benefits for medication, but in a more sustained fashion. Not all movement problems in Parkinson’s disease will respond to medication, and hence not all movement problems will respond to DBS surgery.
Dr Bittar says surgery doesn’t improve things like balance, handwriting or speech. In fact, a patient’s voice can become softer with stimulation. Sometimes DBS can aggravate a patient’s depression, and for that reason, they are advised to see a psychologist or psychiatrist before surgery so their condition can be carefully managed after surgery. For patients who are cognitively impaired, doctors will try to target another area of their brain, so their thinking processes aren’t further affected. Usually the globus pallidus internus (GPi) is chosen instead.
Patients who don’t respond well to levodopa medications are generally not suitable for sub-nucleus stimulation. Surgeons also try to avoid operating on patients in the advanced stages of Parkinson’s disease, who are not likely to have a reasonable outcome.
Professor Malcolm Horne says the need and indications for DBS typically arise in the middle stage of the disease:
Successful DBS is about timing. If it’s too late it occurs towards the advanced stages and it exacerbates the problems of disturbed cognition and neuropsychiatry. On the other hand, it shouldn’t be performed too soon because it exposes the patient to unnecessary interventional risk. As with all procedures, it is most successful when people with Parkinson’s disease are optimally selected and this often means ‘grooming ’ patients to be prepared for surgery when the window of opportunity opens.
There is a trend in Australia and around the world to offer DBS to patients with Parkinson’s disease at an earlier stage … before their physical symptoms take hold … affecting their work and social network.
Dr Richard Bittar, neurosurgeon
Dr David Heydrick’s story
I was 39 and driving home from my neurology practice, and noticed my dominant right finger was slower than my left. A few months later tremor started, followed by micrographia [small handwriting].
Adapted from Dr David Heydrick’s speech on 21 August 2006 at Bethesda, Maryland, USA
After a scan, I canne to grips with my diagnosis of Parkinson’s. Unfortunately, things went from bad to worse rapidly. I couldn’t work, write, drive, button shirts, give talks or even be much of a father to my two boys, including throwing a baseball accurately.
I had reached rock bottom. So in 2005, I went where I originally said I never would: DBS (of the bilateral subthalamic nucleus [STN], staged nine months apart). In hindsight I wish I had done it earlier. I had gone through two miserable years of increasing disability, trying all medications. With DBS, in a matter of months, this was reversed. DBS exceeded my expectations and restored my function and quality of life. I remain off medication. Last month in one week I rode 500 miles [800 kilometres] across Iowa on a regular road bike with my son and the Pedalling for Parkinson’s Team. This would not have been imaginable two years ago.
For about a third of bilateral DBS recipients, the most troubling post-DBS symptom is speech dysfunction. I trade off my voice for tremor control. I can knock out my tremor if I turn up the voltage but I can’t talk. During my bike ride in Iowa I turned DBS off for four hours of intense riding on a tandem bike: the exercise quieted the tremor and my voice was normal. It was a great day. Not all DBS patients have speech dysfunction so possibly it is electrode placement-dependent. I have heard of surgeons testing for voice dysfunction during the surgery, which I would advocate.
My balance was obviously affected. I would reach over to a counter and fall over. This was entirely new and directly related to having bilateral DBS. Better understanding of anatomy relating to balance problems would be quite beneficial for electrode placement and/or programming. Walking different directions on a treadmill and doing tai chi (though not at the same time!) helped with this.
The latest DBS research
US research suggests DBS provides better symptom control than medical therapy for patients of all ages. A recent study surveyed 255 patients, a quarter of whom were aged more than 70 years. Of these, 121 patients had deep brain stimulation, while 134 received the best medical therapy. The results were measured after six months.
Patients who had DBS experienced an extra 4.6 hours a day of good motor control six months after surgery. The DBS group also reported greater improvements in quality of life than those on medical therapy.
The bad news? DBS patients reported 659 moderate or severe adverse events, such as infection from surgery, falls, gait disturbance and dyskinesias. In contrast, the medical therapy patients reported 236 adverse events. More falls were recorded in the DBS group, and behavioural problems, such as depression, confusion and anxiety were higher.





