Lumbar Spinal Stenosis

Who Should Be Fused?
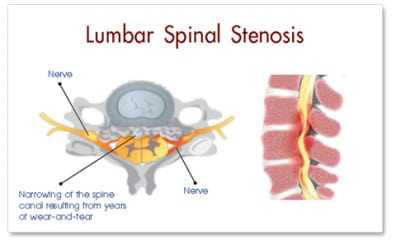
Lumbar spinal stenosis (LSS) is mostly caused by osteoarthritis (spondylosis). Clinically, the symptoms of patients with LSS can be categorized into two groups; regional (low back pain, stiffness, and so on) or radicular (spinal stenosis mainly presenting as neurogenic claudication). Both of these symptoms usually improve with appropriate conservative treatment, but in refractory cases, surgical intervention is occasionally indicated. In the patients who primarily complain of radiculopathy with an underlying biomechanically stable spine, a decompression surgery alone using a less invasive technique may be sufficient. Preoperatively, with the presence of indicators such as failed back surgery syndrome (revision surgery), degenerative instability, considerable essential deformity, symptomatic spondylolysis, refractory degenerative disc disease, and adjacent segment disease, lumbar fusion is probably recommended. Intraoperatively, in cases with extensive decompression associated with a wide disc space or insufficient bone stock, fusion is preferred. Instrumentation improves the fusion rate, but it is not necessarily associated with improved recovery rate and better functional outcome.
Introduction
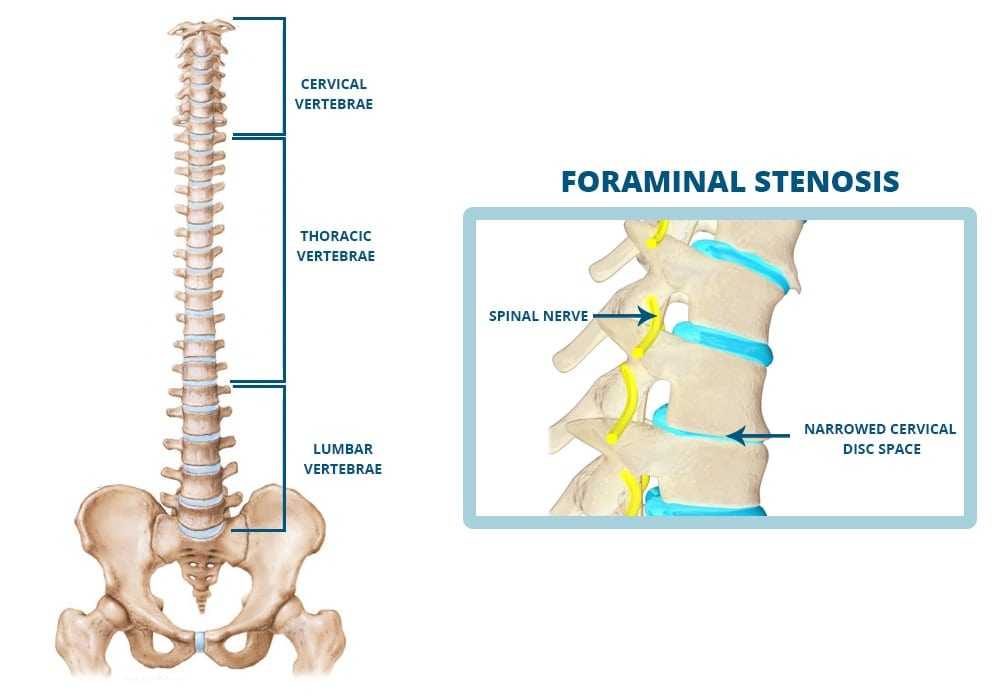
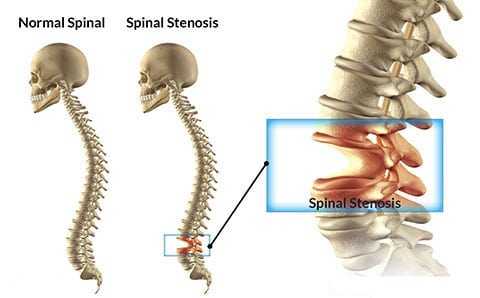
Degenerative joint disease is a degradative process of the joints that primarily involves the articular cartilage . This disease is the leading cause of chronic disability all over the world and usually presents with joint pain, tenderness, stiffness, locking, and effusion . In advanced cases, muscle atrophy, joint instability, or deformity may develop . The arthritic changes in the spinal column (spondylosis) with involvement of the facet joints and intervertebral discs, in addition to these common signs and symptoms, may also cause neurologic impingement . Degenerative process of the spine is usually divided into three phases; inflammatory, instability, and re-stabilization . Although these arthritic changes are more common in the area with greater mobility and pressure like lower cervical or lower lumbar spine, different stages of arthrosis can be observed simultaneously in one region of the spine. Lumbar spondylosis is not synonymous with lumbar spinal stenosis (LSS), but it comprises the vast majority of these cases . Clinically, the symptoms of patients with lumbar spondylosis can be categorized into two groups; regional (low back pain, stiffness, and so on) or radicular (spinal stenosis mainly presenting as neurogenic claudication) . Both of these symptoms usually improve with appropriate conservative treatment . In refractory cases, surgical intervention is occasionally indicated .

Lumbar Disc Herniation versus Spinal Stenosis
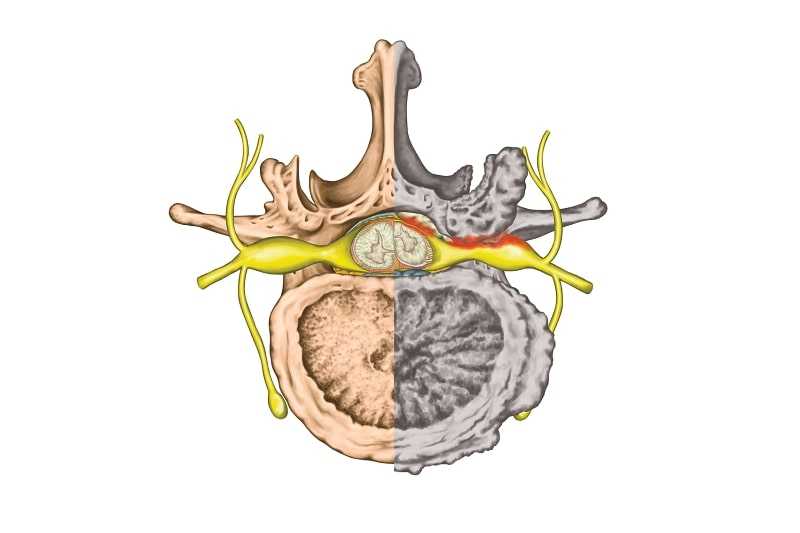
Although traditionally every case of neurologic impingement with involvement of the spinal cord or nerve roots is categorized as spinal stenosis, the patients who present with only intervertebral disc herniation are usually different from those with LSS. In these special cases, the only pathologic finding is herniation of the soft disc without any other abnormality in the adjacent facet joints, ligamentum flavum, or bone. These patients are usually younger and the course of the disease is more acute. Positive straight leg raising test, muscle weakness, and other objective findings are usually more common in these patients. These findings are contradictory to those in patients with LSS who have multiple complaints (inability to walk, inability to stand, or interfere with activities of daily living), but usually no positive objective finding can be detected .
Which Patients Should Undergo Decompression?
The only well known absolute indication for surgical neurogenic decompression in patients with lumbar radiculopathies is cauda equina syndrome (CES). Although CES includes a famous triad of bilateral Achilles areflexia, saddle anesthesia, and sphincter disturbances, these findings are observed in only half of the patients . Therefore, the clinicians should not wait too long to observe all the three features of the syndrome. In other patients with signs and symptoms of LSS, a three-month trial of aggressive conservative treatment is usually recommended, but after this time period, surgery has been found to be associated with significant improvement in all primary outcomes . In ordinary LSS, radicular complaints (other than CES) are usually relative surgical indications, even though most of the authors recommend early neural decompression when the radicular pain is present even at rest . The primary goal of neurologic decompression is to improve the radicular pain. The surgeon should know that the patients who primarily present with a complaint of low back pain may not show much improvement after decompression only procedures even though a relatively severe stenosis might be detected in the imaging studies .
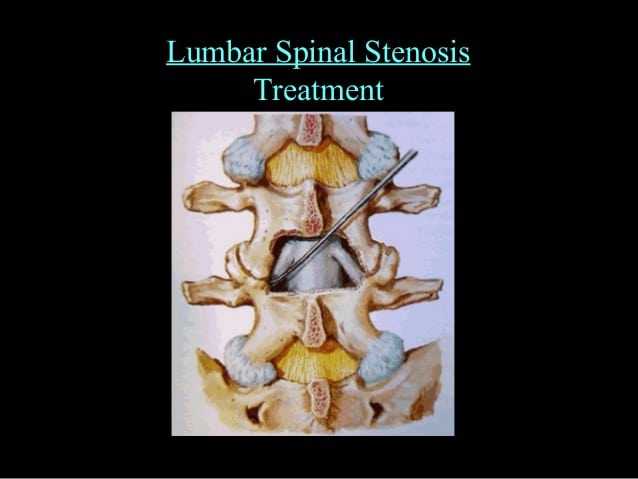
Which Patients Should Undergo Spinal Fusion?
The primary goal of spinal fusion is to improve the regional back pain. Spinal fusion is usually achieved by applying autogenous or allogenous bone graft over the decorticated bone surfaces. Instrumentation may be used to improve the fusion rate and to correct the underlying deformity. Instrumentation may increase the fusion rate (especially in multilevel fusion), but it is not necessarily associated with improvement in the recovery rate. Solid radiographic fusion does not guarantee a successful outcome. Favourable outcome is generally achieved by appropriate patient selection. Appropriate indications for lumbar fusion are usually categorized into two major groups; preoperative and intraoperative indicators. Paying attention to the patient is necessary for making a logistic decision of performing spinal fusion. Before considering these two groups, the clinicians should not forget that in every spinal procedure for achieving spinal fusion, the fusion stage is the most important stage in the whole procedure. If the fusion fails, the world’s strongest implant is doomed to fail.