Modern Spinal Fusion
Patients suffering from severe back pain that does not get better with conservative treatment may become surgical candidates. And if the pain is being caused by a spinal condition such as degenerative disc disease, scoliosis, spondylolisthesis or a spinal fracture, one possible treatment is spinal fusion, which fuses certain vertebrae together to stabilize the spine.
Spinal fusion is a highly documented and proven form of treatment for many patients, but there is something you should know. There is a big difference between traditional spinal fusion and modern spinal fusion. Many innovations and advancements have been developed in the last few years that allow for improved fusion rates, shorter hospital stays and a more active and rapid recovery period.
Here are two big reasons why spinal fusion surgery is better than ever.

Bone Morphogenetic Proteins (BMP)
Traditional spinal fusion often required a bone graft to be taken from the pelvis or the iliac crest of the patient (autograft). The problem with the removal of this bone is that it can be very painful. In fact, around 25 percent of patients who have had this bone graft procedure have some sort of chronic pain associated with the graft site after surgery.
Modern spinal fusion involves using a bone morphogenetic protein (BMP), such as INFUSE® Bone Graft, instead of taking a bone graft from the hip of the patient. BMP is a genetically produced protein with the ability to stimulate a patient’s own bone cells to make more bone.
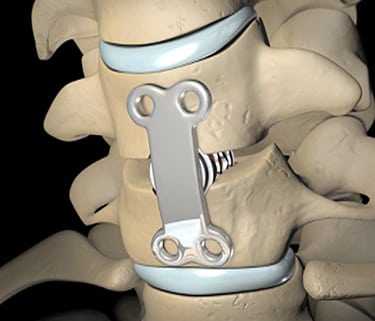
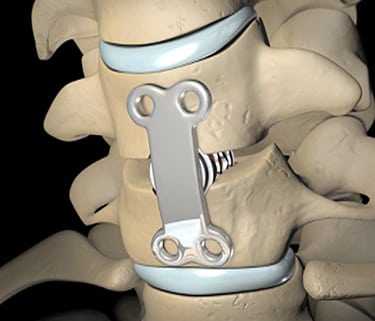
INFUSE® Bone Graft comes to the surgeon in a dry form. During the surgery the circulating nurse re-hydrates the INFUSE® Bone Graft with sterile water. The re-hydrated INFUSE® Bone Graft is placed on a sponge, which is then packed inside a metal device called a cage. This allows for the possibility of a fusion to occur right through the holes in the cage without having to harvest bone graft.
Minimally Invasive Techniques
Surgeons have traditionally used an open approach to perform spinal fusion procedures, which involves making an incision along the middle of the back, stripping large bands of back muscles free from the spine, and retracting the muscles to each side of the opening so that the surgeons can view the spine and easily access the vertebrae for instrument implantation.
Related Article
What You Should Know About Minimally Invasive Spine Surgery
But modern spinal fusion can now be performed using less invasive techniques, making highly invasive posterior fusion unnecessary in many cases. Minimally invasive surgery often involves muscle dilation rather than muscle stripping.
Muscle dilation is achieved by using a series of sequential dilators to separate the fibers of the muscles in your back, making a small tunnel, giving the surgeon a view of your spine through a very small incision. By using these tubes, the surgeon can access the part of your spine where the problem is, without having to make a long incision along those spinal levels.
By allowing surgeons to operate through incisions less than an inch in length and to spare muscle by leaving it virtually intact, minimally invasive techniques can significantly reduce the pain, blood loss, and recovery time associated with traditional open surgery.
As you read this please keep in mind that all treatment and outcome results are specific to the individual patient. Results may vary. Complications, such as infection, blood loss, bowel or bladder problems, are some of the potential adverse risks of spinal surgery. Please consult your physician for a complete list of indications, warnings, precautions, adverse events, clinical results, and other important medical information.