Rheumatoid Arthritis – Cervical Spine

Anyone suffering from Rheumatoid Arthritis for more than ten years has around a 50% risk of developing problems with the cervical spine. The resulting tissue damage and structural abnormalities tend to cause problems in three regions of the spine including atlantoaxial instability, basilar invagination, and subaxial subluxation. The most common is atlantoaxial instability where the first (atlas) and second (axis) vertebrae in the neck no longer move correctly due to ligament and joint degeneration. Atlantoaxial instability causes pain and may lead to dislocation and spinal cord compression. A pannus (localized swelling of synovial tissue) can also form at the atlantoaxial joint causing further compression. Surgical treatment of these problems may involve occipital-cervical fusion in cases where there is no spinal cord compression. Where severe cord compression is evident, however, the patient may require a transoral decompression to remove a compressing pannus and a posterior occipital-cervical fusion with instrumentation to restore stability to the spine following decompression.
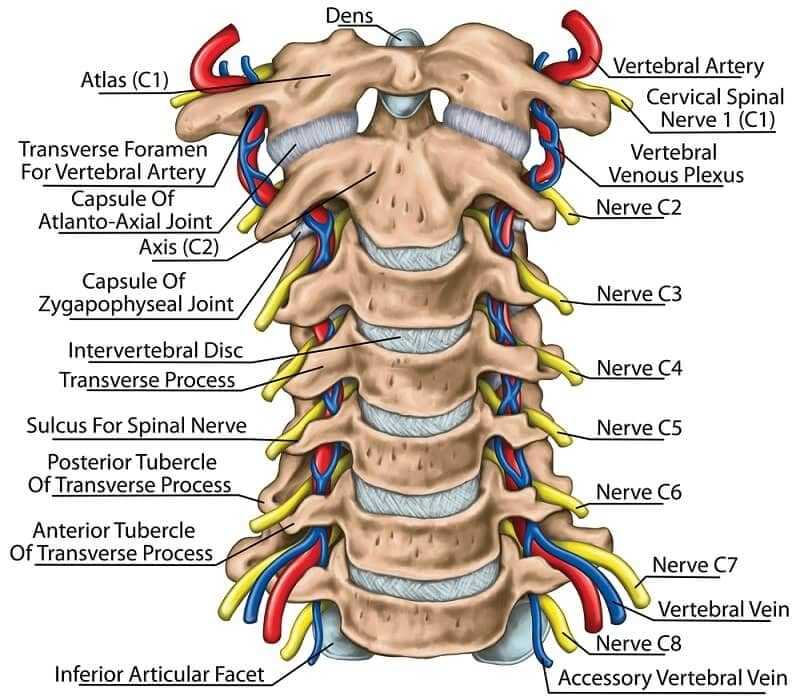
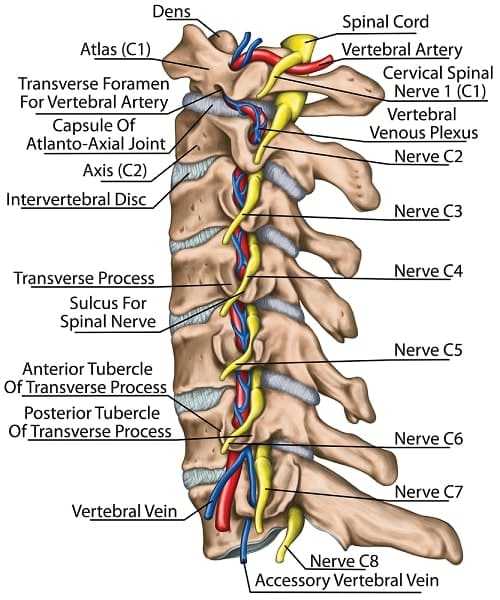
Basilar Invagination
Basilar invagination is a slightly less common effect of Rheumatoid Arthritis in the cervical spine and involves the abnormal ‘settling’ of the odontoid into the spinal column due to instability at the base of the skull. The erosion of the joint at the cranial setting (or superior migration of the odontoid) can cause the section of the spinal cord between the skull and the Atlas to become compressed which can have dramatic effects in terms of mobility, coordination, and sensation. Occipital-cervical fusion is often used to treat basilar invagination, with decompression surgery also indicated where severe compression is evident due to abnormal tissue growth.
Spondylolisthesis in the Neck
Spondylolisthesis in the neck may also occur, whereby the lower sections of the cervical spine (C3-C7) start to slip forward due to the destruction of bone and ligament. This can cause a hunch-like effect similar to patients with ankylosing spondylitis and result in spinal stenosis and instability. Spinal fusion from both the anterior and posterior may be able to correct this in part, or prevent it in patients at risk, but is a difficult surgery due to the complex network of blood vessels, nerves, and other structure in the cervical spine (such as the trachea, thyroid, and oesophagus). If the patient has spinal instability with stenosis then they will require more than just spinal fusion and decompression surgery will be considered. This may involve the removal of osteophytes from the front of the spine through an anterior corpectomy with subsequent strut graft and fusion. If the compression is at the rear of the spine then a laminectomy or laminoplasty is indicated. Severe conditions may require both surgeries. Subluxations of the spine are more likely if a discectomy is performed without spinal fusion, or if a laminectomy is carried out without fusion.