Nonsurgical Treatment Options for Back Pain
Conservative treatment is a term commonly used by spine specialists, referring to nonsurgical options. It should be regarded as a relative concept that compares one treatment method to another, more aggressive, one. Naturally, conservative treatment may not be the best option in every case, and you should examine all your choices before proceeding. Most doctors, however, will first use conservative treatments to resolve back problems. These treatments are usually less risky, though often not as effective, as more aggressive options, such as surgery. Imagine yourself on a ladder where the more conservative treatment options are at the bottom and the more aggressive options are at the top. In most cases you should start with the more conservative options and move up the ladder to the more aggressive ones, if necessary.

At the bottom of this ladder/you will find treatment options such as medications, stretching, heat and cold therapy, aquatherapy, physical therapy, massage therapy, acupuncture, and chiropractic treatments. As you climb the ladder with your spine specialist, you will encounter pain management procedures such as epidural injections, facet blocks, selective nerve blocks, and rhizotomy. Higher on the ladder, you will find minimally invasive surgical procedures, including microdiscectomy and a variety of decompression procedures. The most aggressive surgical procedures, at the top of the ladder, including fusion operations, are used for patients who have exhausted all other, more conservative, treatment options.
Medications
Most people will use medications at some point to relieve their back pain. Even if you have decided to go ahead with surgery, you are probably taking some type of medication to reduce pain and increase function. There are different classes of medications and many different types of medications placed in various categories. In most cases, the medications within a category have similar benefits and side effects. Your doctor will guide you to the appropriate use of these medications and the interaction of one medication with another.
Anti-Inflammatory Drugs
The most common category of medications that your spine specialist may suggest is anti-inflammatory medications, which are divided into two groups: steroidal anti-inflammatory medications and nonsteroidal anti-inflammatory drugs, commonly called NSAIDs. Many NSAIDs have been approved by the Food and Drug Administration, including Arthrotec, Naprosyn, Voltaren, Indocin, Feldene, Clinoril, Motrin, Advil, Ibuprofin, Orudis, Ansaid, Lodine, Daypro, Oruvail, Toradol, Relafen, and Mobic. The basic effect they have on your body is similar, however: they reduce inflammation and swelling, which are the causes of the pain.

Your body has natural mechanisms both to cause and to fight inflammation. You can consider inflammation your friend as well as your enemy, since it is a process that summons white blood cells to the rescue in cases of infections, fractures, lacerations, or even cancer. Unfortunately, inflammation is also a major cause of pain. If you have arm or leg pain that is caused by a herniated disc in your neck or lower back, for example, it is most likely caused by pressure being placed on a nerve, resulting in inflammation in the area. This inflammation causes swelling of the nerve. That, in turn, results in more pressure from the disc. This creates a vicious cycle of more inflammation, along with more swelling and increased pain, which may ultimately result in numbness and weakness. In this case, inflammation is your foe and anti-inflammatory medications are your weapon. The downside of anti-inflammatory medication, however, is that it does not remove the cause of the problem, but only treats its effects.
Side effects are common to all anti-inflammatory medications. Gastritis and sudden gastric bleeding are the most common ones. This is because anti-inflammatory medications block chemicals that are produced in your stomach lining to protect you from gastritis and gastric bleeding. A common recommendation is to take the anti-inflammatory medications with food. This usually reduces the risks of gastric ulcers. Another method of fighting gastric ulcers is to take medications that reduce acids within your stomach. This, however, requires you to take a second pill to counteract the effects of the first one.

Cox-2 inhibitors, such as Celebrex and Vioxx, are a special class of NSAIDs that have a better safety profile for stomach ulcers and gastritis. They were approved a few years ago and became one of the most popular medications around. Unfortunately, after those medications were released, questions arose regarding higher risks of cardiovascular complications associated with their use, and some of them were removed from the market.
Thinning of the blood is another common side effect of some of the anti-inflammatory medications. This becomes an issue if you are considering having surgery. Most spine surgeons will recommend stopping all anti-inflammatory medications one or two weeks before surgery. That’s because these medications can cause increased bleeding, which makes it much more difficult for your spine surgeon to operate. You may also find that you bruise easily, since your blood does not coagulate as efficiently when you are taking anti-inflammatory medications. The medication that is most commonly associated with thinning of the blood and decreasing the effectiveness of your platelet function is aspirin, the antiinflammatory drug with which you are probably most familiar.
Rarer side effects of the NSAIDs include liver and kidney damage. Some patients who have taken massive doses of NSAIDs have suffered kidney failure. Some spine surgeons will also tell you to avoid these medications if you are having fusion surgery because NSAIDs can substantially slow down bone growth at the surgical site, which can lead to failure of the surgery. Because of these potential side effects, most doctors recommend that you do not take anti-inflammatory medications on a long-term basis. If you have been taking these medications for more than one month, your doctor may decide to do periodic blood work to check your liver and kidney functions.
Steroidal anti-inflammatory medications such as cortisone, dexam- ethasone, methylprednisolone, and Depo-Medrol are used much less frequently than nonsteroidal anti-inflammatory medications. This is because steroidal medications are much more potent than the NSAIDs and have many more side effects. They can cause more severe symptoms of gastritis and have other specific and potentially devastating side effects, such as stopping the blood flow to your hip joint. This is a rare complication, but it is still a possibility that must be considered when using this class of medication. For this reason, steroidal anti-inflammatory medications are usually given for only a few days to fight severe symptoms that are unbearable.
Muscle Relaxants
Muscle relaxants such as Valium, Robaxin, Fexeril, Skelaxin, and Soma can reduce muscle spasm and in turn reduce the pain that accompanies many spinal conditions. You may benefit from these medications and rest more comfortably, at least initially, when your symptoms are at their worst. Even though these medications are classified as muscle relaxants, their specific action for reducing pain is not entirely understood. It is hypothesized that they result in drowsiness, which in turn can relax your muscles.

This class of drug does not affect the cause of your problem, but only improves your pain while the medication is in your body. Still, muscle relaxants can be effective if you recently injured your back. Most injuries that result from lifting or abnormal movements are caused by muscle spasms and local inflammation. For this reason, muscle relaxants can be helpful in acute injuries, usually for only a few days after the injury has occurred. If your pain lasts more than a few weeks, muscle relaxants will be ineffective in providing you any long-lasting improvement. This is because most injuries and pain that last beyond a few weeks are not caused by muscle strain alone.
The various muscle relaxants have different potencies, potential for addiction, potential for causing drowsiness, and duration of action. Your doctor will choose the appropriate medication based on his own familiarity with the medication, his experience, and his knowledge of side effects and drug interactions.
Pain Medications
Pain medications such as Vicodin, Percocet, Vicoprofen, and Norco are also commonly prescribed for back pain. Most pain medications are derivatives of opiates and other narcotics, such as morphine and codeine. They directly fight chemicals that produce pain, and most have some addictive potential. There are two different components to addiction. One is tolerance and the other is dependency. Tolerance describes that fact that your body learns to process the medication more efficiently and, as a result, you may not feel the same beneficial effect after a few weeks or months of using it. For this reason, you may end up needing higher and higher doses to get the same pain-relieving effect. Dependency means that your brain gets used to having these medications and you can develop a drugseeking behavior that is not in response to the pain.
There is a balance that must be maintained between pain relief and overuse of these medications. Your doctor can guide you in their appropriate use. In fact, there is a medical specialty dedicated to pain management. Doctors who specialize in pain management are usually anesthesiologists who have completed one year of specialized training in pain management. Your spine surgeon may refer you to such a doctor if your need for pain medication is complicated, or in cases where dependency and tolerance have developed.

As with other classes of medications, many different pain medications are available and each one is available in various dosages. Some are fastacting, for severe, sudden pain; others are taken periodically, every few hours; and still others are available in the extended-release format and are used daily. Pain medication patches are also an option. Doctors try to prescribe the least amount of medication to control pain and maintain function. The stronger the medication and the longer you have taken these medications, the higher your chances of encountering complications.
Your physician will be guided by the information you have provided him. That’s why it is so important to give your doctor accurate information. If you underestimate and describe your pain as mild, your doctor will attempt to use weaker medications to relieve your pain, which can result in undertreatment. If you overestimate your pain, however, and complain of severe, debilitating pain, stronger, more potent medications will be used. Keep in mind that you have the responsibility to convey accurate information so that appropriate medications are prescribed to you.
If your doctor attempts to decrease the strength of your medications, he is being conscientious and is practicing good medicine. Some pain management doctors place their patients on a strict schedule to avoid overutilizing these medications. They may even ask patients to sign a formal contract before they begin treating them. These contracts dictate the rules that are followed when using pain medications and the rules regarding medication refills and follow-up appointments.
Sleep Medications
Pain not only causes musculoskeletal dysfunction; it also has psychological consequences, such as depression, mood changes, and sleep disorders. Many patients who complain of pain have difficulty sleeping. Lack of sleep by itself can lead to an array of other consequences and increase your sensitivity to pain. Patients who get a good night’s sleep can cope with pain much more effectively. Your doctor may consider prescribing sleep medications such as Dalmane, Restoril, or Ambien for a short period if you need them. Sleep medications do have addictive potential, however, and may cause more harm than good on a long-term basis. Your doctor can decide which medication is appropriate for you and how long you should use it.

Nerve-Stabilizing Medications
If you are suffering from nerve pain, which can be characterized by numbness, sharp discomfort, or abnormal sensation that radiates to your arms or legs, nerve-stabilizing medications can be of some help. The exact mechanism by which they reduce this type of pain is still unknown, but animal studies have shown that these medications reduce pain produced by nerve dysfunction. These medications are also used in patients who have diabetes-related nerve pain. Examples of such medications are Neuron tin (gabapentin), Lyrica (pregabalin), and Elavil (amitriptyline). They are used for other disorders as well and should be used with caution. Neurontin is used to suppress seizures, but stopping the medication suddenly may actually result in a seizure. Elavil, on the other hand, is used to treat depression. Stopping it abruptly may result in depression and worsening of your pain. It is difficult to predict which of these medications will work best for you and, unfortunately, it often requires trial and error to find out.

Topical Medications
Topical medications can act locally or be absorbed through the skin and have the same effects throughout your body Like pain medications, they can also be delivered by patches. Opioid pain patches are usually reserved for patients on high amounts of medications. An example of this type of delivery system is the Duragesic patch. It releases a constant flow of the opioid drug into the body and eliminates the ebbs and flows of the drug that occur when you take the medication orally. Other types of patches include one that delivers a numbing medication—lidocaine (also used by dentists)— locally to the area of pain.
The most common of these types of patches is the Lido- derm patch. It can be applied once daily to the area of pain, but should be removed after twelve hours to avoid excessive delivery of the drug to your body. Even after you remove the patch, the effects of the medication will last for another twelve hours. If you are not allergic to the drug in the patch, you may derive benefit from using this medication for back and neck pain. A Lidoderm patch will not provide any benefit for nerve pain radiating to your arms or legs, since it only acts locally. Furthermore, these patches only treat the symptoms of your problem, not the cause. This patch is relatively safe, however, with very limited side effects.
Also available are various creams that can treat pain locally. Common over-the-counter creams include brands like Icy Hot, Bengay, and Capsin. These creams act locally and produce a sensation of heat and other stimuli that divert the sensation of pain from your brain. They can be effective for mild pain and have low rates of side effects.
Other Non-InvasiveTherapies
These modalities of treatment are the next step up the ladder after medications. For the most part, they do not have irreversible effects, and at least three of them (physical therapy, Pilates, and yoga) involve strengthening your muscles to provide better support for the other structures of your spine. Let’s examine them now one at a time.
Physical Therapy
Physical therapy is the most common and least controversial treatment for back pain. What is physical therapy? It usually prescribes movements of your muscles and back in strategic ways to strengthen specific muscles, along with improving your posture and increasing the flexibility of your joints, tendons, and muscles. Most commonly, physical therapy is provided by a physical therapist, but chiropractors or other practitioners may also do it. Even though most back pain will resolve on its own, physical therapy can expedite your recovery and possibly also help you avoid recurrent episodes of back pain.

One of the basic concepts of physical therapy is to strengthen the back muscles so that they can provide more support for the other structures within the spine; stronger muscles can absorb the forces that affect the discs, joints, and ligaments of your spine. Endurance training is another important aspect of physical therapy. Your back muscles must provide continuous unrelenting support to your spinal column, while maintaining flexibility at the same time. No wonder that they tire, placing your spine at risk for injury. The longer your muscles can maintain their support, the less risk you will have for reinjury. This is called endurance. Flexibility is yet another key attribute that can be improved with therapy and exercise. The more flexible your muscles and tendons are, the more they can support and protect you in the different positions in which your spine may be placed.
Generally, women have problems that result from weak muscles, as compared with men, who have problems that are related to endurance. Most women will benefit from programs that strengthen their muscles and most men will benefit from programs that increase the endurance of muscle activity.
Physical therapists and other practitioners also offer additional treatments that include heat therapy, cold therapy, ultrasound, interferential muscle stimulation unit, massage therapy, acupressure, reflexology, and cold laser. These passive modalities are generally used during the initial period after the injury to help you cope with the pain. Most of these therapies increase local blood flow or decrease inflammation. Generally, they do not have long-term benefits, and you can expect to see improvement of your symptoms for only a few hours.

Aquatherapy (water therapy) is another modality that uses the basic principles of physical therapy Aquatherapy is performed in a pool, so that the water in effect reduces your weight, resulting in less stress to your joints when you perform exercises. You may feel protected in the water, which can have a psychological benefit, allowing you to perform more strenuous activities.

There are a few basic concepts that you should follow with every therapy program. You should always distinguish between deep, sharp pains as compared with muscle soreness, which may result from decon- ditioned muscles. You should also set a goal for your exercise program and should avoid going beyond that goal initially. As you start a physical therapy program, you may not feel that you have accomplished anything until a day later. At that time, you may feel intense muscle soreness that can actually slow you down. Because of that, most physical therapists will recommend that you start slowly and increase your level of activity over a few sessions. You should also avoid jerking movements or sudden extreme activity. Make your movements controlled and concentrate on the movement before you begin it.
Initially, perform a routine only for a few minutes. Increase that slowly over the next few sessions. If you begin an aerobic exercise, you may not be able to engage in it for more than two or three minutes at first. The next time, increase it to five or ten minutes, and then increase it to fifteen minutes. This can avoid any unnecessary frustration or the feeling that you cannot perform the exercise. This can also give you a sense of accomplishment once you have achieved your goal, at which time, with the blessing of your physical therapist, you may decide to surpass your goal altogether. Always remember, twisting is the enemy of your back and should be avoided in any type of exercise program unless it is slow and controlled.
Chiropractic Manipulation
The principle underlying chiropractic manipulation is that small misalignments of the spine can cause pain locally. Although their claims are not well accepted, some chiropractors argue that the key to other illnesses (including diabetes and childhood ear infections) lies in the spine, and that the correction of these misalignments can treat or even cure some medical conditions. Unfortunately, these misalignments often cannot be detected by X-ray unless they are severe, but they can be felt by a chiropractor. Practitioners of this therapy believe that manipulation of the spine moves the joints, tendons, and ligaments into their appropriate positions.

Chiropractic manipulation often produces a distinct sound and a sensation of relief, which is the hallmark of this type of therapy. The downside of chiropractic treatment is that the benefit only lasts a few hours and you may require long-term treatment to find lasting relief. There have been reports of catastrophic complications when patients with fractures or tumors have had chiropractic manipulation. Chiropractors undergo three or four years of training to reduce these risks as much as possible.
Related Articles
Can a chiropractor help a herniated disc ?
Does Chiropractic Treatment Work?
Acupuncture
Acupuncture is an age-old technique that relies on the placement of tiny needles in specific locations to reduce pain and dysfunction. These locations have been mapped by an ancient philosophy that is still used today. The exact mechanism by which acupuncture reduces pain is unknown and much controversy exists regarding its effectiveness for long-term pain relief. One theory is that the tiny needles placed in the skin redirect the pain signals and divert them away from the brain. Another theory suggests that the needles cause the release of endorphins (naturally produced morphine within your own body), which in turn reduces pain. Consider this to be like asking your own body to produce pain medication locally.

Acupressure uses a similar concept; focal pressure in specific areas can redirect pain signals and produce beneficial effects. There are no definitive scientific studies demonstrating the benefits of these treatments. They pose a low-risk option, however, and are at least worth a try.
Pilates and Yoga
The exercise techniques of Pilates and yoga, although they have been around for decades and centuries, respectively, have recently become popular and offer promising results to chronic back sufferers. They instruct participants in controlled movements of muscles that are not used during routine daily activities. These are called core exercises and promote the development of the muscles that are responsible for balance and posture. Yoga also uses powerful mental techniques and meditation for relaxation.

In moderation, these exercises can be helpful; extreme twisting and bending, however, can aggravate or even cause injury. As with any other exercise, start slowly and increase the intensity to a point that is comfortable for you. Some instructors may motivate you to reach above and beyond your goals, which may result in further injury.

The unique benefit of yoga is, as mentioned above, its use of meditation and mental relaxation. Otherwise, it uses the same basic principles of strengthening, stretching, and endurance training common to other types of exercise programs. Pilates also employs similar concepts but through the use of specialized equipment that utilizes the weight of your own body to produce resistance for muscle activity while avoiding significant movement. The exercises focus on muscle strengthening and endurance training while also emphasizing flexibility and stretching. Pilates uses all the principles of physical therapy with the added advantage of promoting weight loss. Pilates is not for you, however, if you have recently had a flare-up of back pain or have suffered a new back injury. Pilates and yoga should be used as a way of life when recovering from chronic back pain or in maintaining a healthy back.
Pain Management Procedures
Better understanding of the causes of back pain has led to the development of various modalities of pain management. Your pain management specialist has been trained in injection techniques and has knowledge of the most potent pain medications.
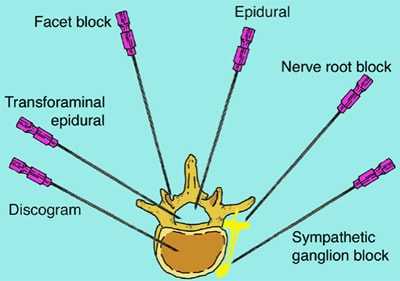
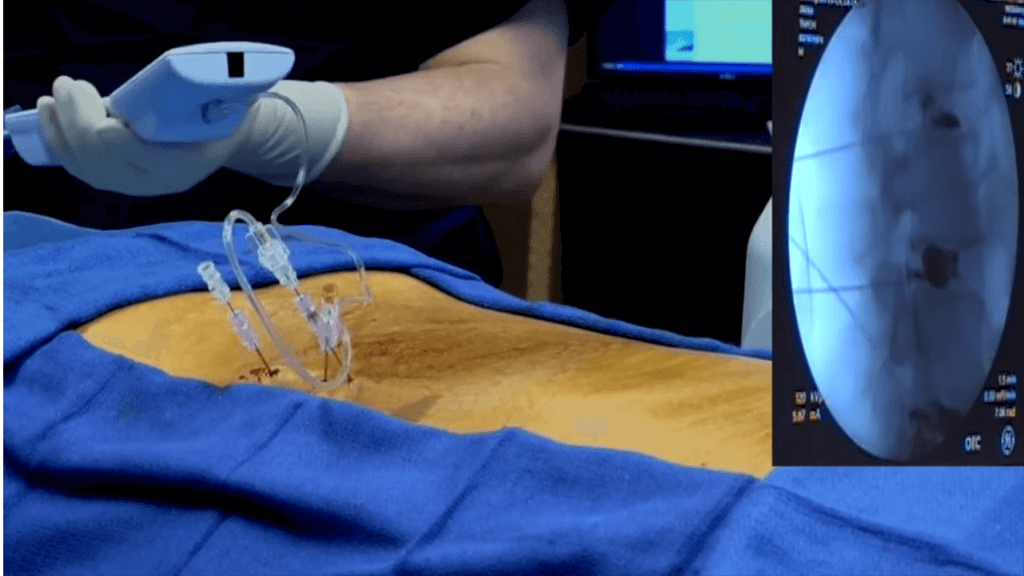
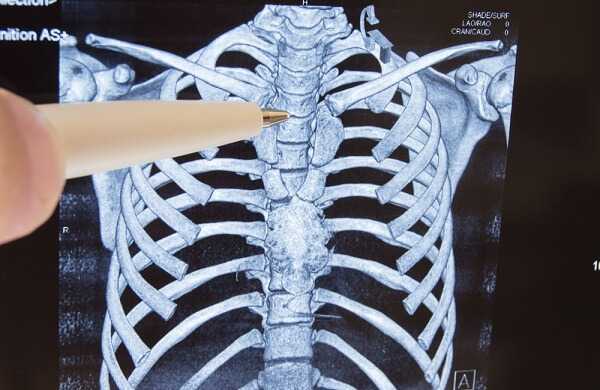
Epidural injections are one of the most common types of treatment offered by pain specialists. These are performed by placing a needle in a specific area of your spine and injecting steroid medications to combat inflammation. Other types of injections include facet blocks and discograms, which are performed either to diagnose or treat your condition. Most of these procedures are performed under X-ray visualization. Commonly, when performing one of these percutaneous procedures (i.e., through the skin), your spine specialist will use a fluoroscopy unit —a machine that allows him to take an X-ray picture and immediately see the image on a television screen. It also permits these X-ray pictures to be taken from various angles, which allows the physician to place a needle with great accuracy in almost any area of your body.
Epidural Injection
Epidural injections are performed by pain management specialists to treat back pain that radiates to your arm or leg. They are used to treat the pain caused by cervical, thoracic, and lumbar disc herniations, cervical spinal stenosis, and lumber spinal stenosis. You may have heard of epidural injections administered during childbirth. Epidural injections for back problems are somewhat different, since they are not meant to numb your extremities and there is no need to place a catheter in the spine. They simply deliver a small amount of steroid medication such as Celestone, cortisone, or Depo-Medrol locally around the nerves with a needle, which is removed immediately after the injection. If, for example, you are suffering from spinal stenosis or a disc herniation, your nerves are inflamed and swollen. Oral medication is distributed throughout your body and some of that medication is delivered through your blood to the area of inflammation. An epidural injection, by contrast, can deliver the medication with pinpoint accuracy to the area around the nerve, which results in much higher concentrations of the medication where it is needed most.

Most pain management specialists will perform epidural injections in an operating room under fluoroscopic guidance. Some specialists perform these injections in their office without the fluoroscopic imaging; the accuracy of the injections performed without fluoroscopic imaging, however, is usually lower. There are no specific recommendations in regard to the number of epidural injections that can be given or how often they should be administered. A general guideline is to perform a series of three injections, one week apart. This sequence usually insures adequate delivery of the medication to the affected area.
You can ask your doctor to make you drowsy before the injection so that you are very comfortable throughout the procedure. Expect to walk immediately afterward, with some soreness locally in the area of the injection. You may obtain benefit from the injection within one or two days. How long an injection will improve your symptoms is unpredictable. At best, the effects usually wear off after a few months. So, even though epidural injections have a relatively low rate of side effects, you should carefully consider your options because they don’t work on all patients and their effects are usually temporary. Epidural injections have not been shown to change the final outcome if surgery is actually needed. The injections can, however, delay the need for surgery for a few months.

A common misconception is that epidural injections can weaken the bones in your body. This is generally not the case with epidural steroid injections, since the amount of medication is low and they are usually performed only a few times. By contrast, if you are using oral steroids to treat other conditions, such as lupus or rheumatoid arthritis, the medication can cause deterioration in bone density.
Selective Nerve Root Block
Selective nerve root blocks are usually regarded as a special type of epidural injection. The specialist administering a nerve root block injects cortisone, as in an epidural injection, as well as a numbing medication, around one single nerve into the neural foramen. Selective nerve root blocks can decrease pain if the area of concern is localized to one single nerve. Selective nerve root blocks can also be used as a diagnostic tool. If your spine surgeon has a question regarding the specific nerve that is under pressure, then selective nerve root block may provide the answers.
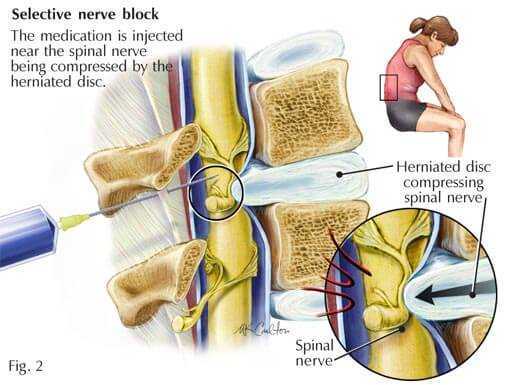
For example, if your spine specialist suspects that a disc protrusion is placing pressure around the L4-5 neural foramen, a selective nerve root block at that level can confirm or contradict the diagnosis. This can be very helpful before surgery and may guide your spine surgeon to perform surgery on one specific disc level instead of multiple levels. In some cases, therefore, selective nerve root blocks can provide information that substantially increases surgical success rates.
Facet Block
Facet blocks are another common pain management procedure that can be used to diagnose or treat back pain. The facet joints, as we have seen, are the small joints in the rear of the spine that connect the vertebrae to one another. Just like any other joint in your body, they can develop pain and stiffness. Arthritis can cause the facet joints to enlarge and develop irregular surfaces, which can lead to pain when you attempt to move your spine. Inflammation of the sensory nerves attached to these joints can also cause pain. The location of these very small nerves is known and inflammation can be reduced by steroid medications delivered next to them. Facet blocks are performed in a manner similar to epidural injections, including the use of fluoroscopic guidance. Sometimes anesthetic medications are injected into the facet joints to see if your pain is originating from those joints. If you have immediate pain relief after an injection of an anesthetic medication in and around the facet, we can conclude that your pain is originating at least in part from the facet joint.
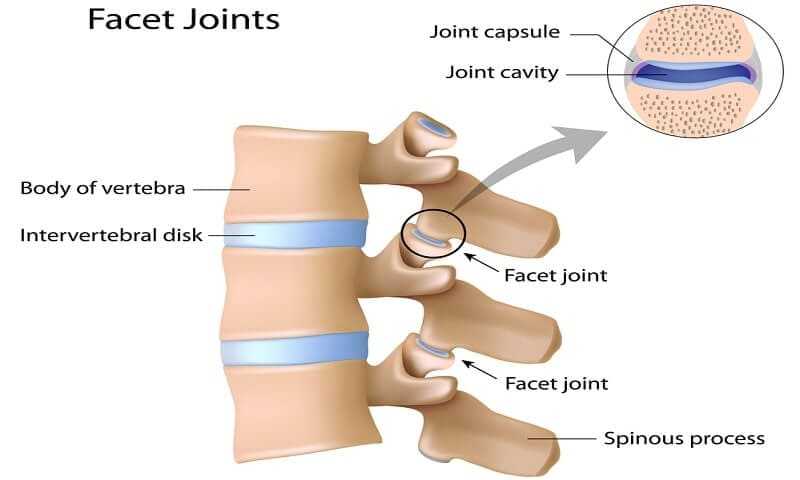
To you, a facet block will feel just like an epidural injection, since the only difference between the two is the location of the injection. In the operating room, you will probably be given sedatives before the facet block is performed. The skin is numbed and the needle is placed under fluoroscopic (X-ray) guidance. The needle is advanced to and around the facet joint. An injection, usually to the neck, mid-, or lower back, is performed, and then the needle is removed. An experienced pain management specialist can usually administer these injections in one or two minutes. Like epidural injections, they are performed in a series of two or three, a week apart. More than one joint can be injected at the same time if an MRI or CT scan has shown irregularity or enlargement of multiple facet joints.
Rhizotomy
If you have already had facet blocks performed and found obvious improvement in your symptoms, then rhizotomy may be the next logical step in treating your back pain. Rhizotomy destroys the small nerves that are located next to the facet joints and that transmit pain information from the facet joints to the brain. This procedure is performed in a manner similar to a facet block except that heat is applied for a few minutes with a small needle next to the nerve around the facet joint. Rhizotomy blocks the pathway for the sensation of pain that originates from the facet joints. The drawback of rhizotomy procedures is that the effect does not last forever. These nerves can regenerate and the pain may recur. Some spine specialists suggest repeating the rhizotomy procedure every six months to control your pain. The effects of repeated rhizotomy procedures may be longer-lasting than the first one.
Related Article
Discogram
Discograms are often done purely as diagnostic tools. If you and your spinal specialist are in search of the cause of your back pain and for the specific disc that is causing it, then a discogram may be the next logical diagnostic test.
It is known that a normal disc will not produce pain when a needle is placed in it and fluid injected into it. By contrast, an abnormal disc will usually produce pain—and may reproduce the back pain you feel on a daily basis—when fluid is injected into it, increasing the pressure within the disc or irritating the tear if one is present. If you and your surgeon have decided to proceed with a surgical fusion of your spine, your surgeon may request a lumbar discogram prior to the surgery. This will provide information regarding the specific discs that are causing your back pain, thereby preventing your surgeon from fusing unnecessary disc levels. The goal is to perform the least invasive surgery while achieving the best surgical outcome, most improvement of symptoms, and the longest-lasting effect.
Related Article
Discograms can be performed in the cervical or lumbar spine; in the cervical spine, however, they pose a much higher risk due to the difficulty of approaching the disc without causing injury to major vessels and nerves, the esophagus, the trachea, or the spinal cord. In the lumbar spine, the needles are placed obliquely to avoid injury to nerves and to the abdominal contents. Since in most cases, a discogram will be performed on the lumbar spine, I will describe a lumbar discogram.
Under the guidance of fluoroscopy, a needle is placed within each of three or four discs. Once all the needles are in the discs, fluoroscopy confirms their positions. A dye that increases the pressure within the disc is injected. Your doctor will then ask you two very important questions. One question is whether you feel pain when he is injecting the dye, and the second is about the quality of the pain. The presence of pain alone does not make a discogram positive. In order for a discogram to be positive, the test must reproduce the same type of pain that you feel every day This is called a “concordant positive discogram.” A painful disc that does not reproduce the same quality of pain is a negative discogram. The test will usually be performed over a few disc levels. Your doctor will want to test the reliability of the discogram by placing a needle and dye in a disc that appears normal, as well as a disc that appears abnormal. Your doctor would expect a painfree disc if the MRI on that specific disc level is normal. In contrast, pain should be reproduced at the disc level that looks abnormal on the MRI.
Some doctors will obtain a CT scan after a discogram to examine the internal structure of the disc. More information can be obtained from a CT scan after a discogram has been performed. This is called a CT-discogram. A common finding on a CT-discogram is an annular tear, or a tear in the outer covering of the disc, which can cause pain. If there is a tear in the annulus of the disc, the dye that is injected within the disc during the discogram can be seen seeping out of the disc through the annular tear.
Even though many surgeons do use a discogram as a diagnostic tool, some spine specialists do not believe in the accuracy and reliability of this test. This controversy notwithstanding, the discogram is the only test that can prove that a disc is causing your back pain. As we have discussed, not all discs that look abnormal on an MRI will cause pain, and therein lies the value of a discogram. The discogram itself provides information regarding the severity as well as the character of the pain, and the CT scan provides the visual information regarding the integrity and shape of the disc.
Conversely, even if you have a positive discogram, your MRI study may show relatively normal images of your discs. This can pose a challenge to your spine surgeon in choosing the appropriate treatment plan for you. In most cases, if the puzzle does not fit, it’s always safer to go the conservative route. In cases where the MRI is normal but the discogram reveals positive concordant pain, most spine specialists would suggest avoiding surgery and trying further conservative treatment to reduce pain and increase function.
Intradiscal Electrothermal Therapy (IDET)
In intradiscal electrothermal therapy (IDET) the outer envelope of the disc is heated and, in theory, a tear in the annulus is closed and the tiny nerves that transmit pain sensation from the disc to the brain are burned. Three or four years ago, this procedure was extremely popular for treating lower back pain and was regarded as a minimally invasive procedure with relatively low risk.
The procedure is done in the operating room under deep sedation. Without sedation and anesthesia, the procedure would be extremely painful and could not be tolerated. The approach is similar to that of a discogram in that a needle is placed within the disc space. After placement of the needle, its position is confirmed using fluoroscopy, and a wire is passed through the needle into the center of the disc. As the wire passes within the disc, it comes very close to the outer covering of the disc. The wire is then attached to a machine that heats it up, theoretically burning the small nerves around the annulus of the disc. Following this procedure, the patient is initially required to use a brace and then to do specifically recommended exercises.
https://www.youtube.com/watch?v=G-wPS7HTiMI
When IDET was first introduced, the only research articles available were written by the physicians who developed the procedure. The initial success rates recorded by those physicians were approximately 80 percent. As more research articles were introduced into the scientific community, however, it was found that the success rates were lower than those initial reports had documented. A careful search for recent studies on IDET outcomes indicated that it does produce moderate improvement in back pain.
There are conditions that will prevent you from having an IDET procedure, such as a disc herniation or radiation of pain from your back to the leg. If you have leg pain, it may be due to a herniated disc that is placing pressure on the nerves that travel to your leg. In that case, it is not advisable to undergo an IDET procedure, since there is a risk that the wire that is advanced into the disc might enter the spinal canal itself.
The IDET procedure should only be performed after a discogram has revealed concordant pain. Furthermore, the best results have been seen in patients who have only one abnormal disc. The rate of success decreases if you have multiple discs that are abnormal. Since the failure of the IDET procedure does not prevent you from having a more aggressive treatment such a lumbar fusion, however, you may consider this procedure as another option to treat your back pain.
It is worth noting that some spine surgeons have abandoned IDET procedures altogether because they do not provide reliable or consistent outcomes. In the geographic area of my practice, most spine surgeons have stopped performing IDET, and I have not performed this procedure for the past few years.
Summary Remarks
If your pain resolves with the conservative modalities that we discussed in this article, bravo! That is a wonderful outcome. You have succeeded in achieving the goal of defeating your back pain. If your pain has not decreased, however, you may want to consider climbing the ladder to more aggressive treatment options. Next, we will explore those surgical options, investigating their benefits and risks.