What is the best injection for knee pain
The knee is the most commonly injured joint in people who are physically active. The majority of people who presented themselves to my clinical pain practice due to chronic joint pain were nearly always people with some type of knee malady. This monograph will be an explanation of what I believe to be the best knee injections.
I am going to share with you my approach to the best knee injections. This is an approach that took me over 20 years to perfect as I performed hundreds of knee injections every year in my practice. It is the technique that evolved as I carefully listened to my patients reports of relief (or lack of it), evaluated the medical literature, and pondered the physics of injection technique. I believe you are going to learn some things that you have never heard before (even if you are a health care practitioner).
The Anatomy of The Knee
The knee is a mechanically “at risk” joint. What I mean by that is that the very structure of the knee places mechanical forces on it that can amplify “wear and tear.”
You can think of the mechanical disadvantage of the knee this way…2 long poles attached by cords attempting to limit the backward and forward…side to side motion at the ends where the 2 poles meet…that’s the knee.
When the knee is involved in activity it moves in a multi-planar way (though its’ major motion is like a “swinging hinge”). In motion, all attachment and cartilage tissues of the knee are stressed. When standing erect the knee rotates slightly, “locks out,” and handles its’ weight load with a minimum of ligament and tendon strain.
The knee also has two curious interior structures called menisci (meniscus in the singular). The menisci guide the synovial surfaces of the knee and help decrease the “backward and forward – side to side” motion of the knee. They stabilize the sliding surfaces, disperse friction, and cushion the knee. They are made of fibrocartilage (similar to the substance of the outer ring of a vertebral disc).

Even at bedrest the knee is moving (just ask a friend who has had knee surgery). There is no possible way to eliminate motion of the knee without fusing it. Fusion is a surgical procedure where the femur (upper leg bone) and tibia (lower leg bone) are surgically made into one long pole.
Although this may reduce or eliminate knee pain, the additional stress on other joints (namely the hip) often results in earlier hip dysfunction necessitating eventual surgery of the hip.
Even bracing of the knee gives it little support. Orthopedic studies done on football offensive lineman (the largest people in professional football) show that a knee brace works by reminding the lineman to reduce the strain on their knees by changing the way they block. It offers little measurable supportive help.
The Physiology of The Knee
The knee is a “swinging-hinge” mechanism. The actual major motion is in the form of an arc. It is really an eccentric arc that places stress on different structures within the knee at different phases of its motion. The study of this movement is called kinesiology.
In the standing position the knee ligaments (which attach one bone to another) and tendons (which attach muscle to bone) are at their least stress. The major stress standing is compressive and is applied to the cartilage located on the end of the tibia and femur (called synovial cartilage).
As the knee begins to bend, the patellar tendon tension (the patella is the “knee cap”) begins to rise first. As motion continues tension in all ligaments and tendons builds to reach maximum stress at the fully bent position (the “squat”). A full squat places the greatest tension on the structures of the knee.
Ironically, the knee is the most vulnerable to external forces in its least stressed position, the partially bent knee (5 or 10 degrees of bend). Presumably, this position allows external forces to separate the knee compartments easiest due to ligament and tendon laxity.
Ligament shearing remains a major mechanism of injury in sports. More recent orthopedic surgical techniques utilizing cadaver ligament and tendon transplants (called allograft transplants), as well as tendon transplants from one part of the same person’s body to another (called auto graft transplants), have improved recovery from cruciate ligament tears.
Ligament looseness (called “laxity”), tendon looseness (also “laxity”), and loss of cartilage of the knee are usual with the aging process. Injury of the knee, at an earlier age, accelerates the aging process of it. If a human being lives long enough, especially one who has had an active athletic lifestyle, they will develop some category of knee problem.
Conditions That Respond to Injection
The following conditions of the knee have been found to have the chronic pain they cause reduced by knee injections:
- Degenerative Joint Disease of the Knee (this is the most common reason for knee injections).
- Patellar Condromalacia (a wearing away of the cartilage on the under surface of the knee cap).
- Rheumatoid Arthritis of the Knee
- Other Autoimmune Conditions of the Knee
- Select Ligamentous and Tendinous Conditions of the Knee
- Select Cystic Conditions of the Knee Cartilage
- Select Tumorous Growths of the Knee
IT IS IMPORTANT TO NOTE, AT THIS JUNCTURE, THAT KNEE INJECTIONS ARE PREDOMINATELY USED FOR THE CONTROL OF PAIN AND DO NOT SIGNIFICANTLY ALTER THE ON GOING DETERIORATION OF THE KNEE FROM A CHRONIC CONDITION.
Medications Used in the Knee Injection
The following medications are often used alone or in conjunction with each other when performing a knee injection:
- A local anesthetic agent (such as Lidocaine)
- An injectable corticosteroid (such as cortisone)
- A skin preparatory agent to disinfect the skin prior to injection
- A skin anesthetic agent to reduce the pain of the injection
The medications i used were as follows and for the following reasons:
1) Marcaine 0.25% solution in a multidose vial:
I liked this long acting local anesthetic agent because it gave very rapid pain relief (within minutes) and persisted until the other medicines in the “mix” could begin to work. If you look at the literature about this anesthetic agent it is not officially approved for joint injections. This is because it can cause cartilage damage when used as a continuous infusion into the joint (such as after surgery) when using the O.5% concentration.
In my mix we used the 0.25% solution and never more than 1cc (mixed with 2 ccs of other fluids). This very low concentration of Marcaine never caused any reactions in any patients in over 26 years of practice.
2) Depo-Medrol 40 mg per cc multidose vial:
This is a moderate acting corticosteroid that is a suspension (there are tiny micro-granules of steroid) which prolongs the duration of action of the medicine. Although there are many side effects that can occur with the systemic administration of corticosteroids, when given into a joint the systemic absorption is much less and subsequently the side effects are less also.
This substance is an anti-inflammatory and will “calm down” the swelling that can occur in certain knee conditions. Our dose was 1 cc (or 40 mg) mixed with 1 cc of Marcaine and another 1 cc of a substance called Sarapin.

3) Sarapin is a natural anti-inflammatory made from the Pitcher plant.
I used a multi-dose vial of this substance and added 1 cc of it to my injectable mix. It has no side effects and never provoked any reactions in over 26 years of giving joint injections.
THEREFORE, THE INJECTABLE MIX THAT I USED IN MY PAIN MANAGEMENT PRACTICE FOR OVER 26 YEARS WAS A MIXTURE OF 1 CC OF MARCAINE 0.25 % TO 1 CC OF DEPOMEDROL 40 MG PER CC TO 1 CC OF SARAPIN. THE TOTAL VOLUME FOR THE KNEE INJECTION WAS 3 CC.
I believe that the combination of local anesthetic (giving immediate relief) with 2 anti-inflammatories (the Sarapin diluting and amplifying the Depomedrol) was the reason why we had such profoundly positive results with our knee injections. I cannot recall any patient not obtaining relief with our injection mix nor do I recall any serious side effects in nearly 3 decades of performing this type of injection.
Equipment Used in The Knee Infection
We also used a unique array of equipment when we performed knee injections. Over the years I noticed that physicians who performed this type of injection were accustomed to using a fairly heavy 18 or 20 gauge needle. The patients would often complain about their past experience with knee injections that, although they obtained relief, the actual needle insertion was excruciating.
I decided to use a 27 gauge Titanium needle for knee injections (a much thinner needle). Most thin needles are short as they tend to bend easily when thin. However, Titanium is a stronger metal and does not bend so easily even when very thin. I was able to find 1 1/2 inch Titanium needles that could easily traverse the distance from the skin surface to the interior of the knee.
As long as I did not have to remove fluid from the knee (a fluid that is usually like pancake syrup) I could use the thinner needle for injection only. If fluid had to be removed I would have to resort to the thicker 18 gauge needle as you cannot pull out thick fluid with a 27 G needle.
I also used 3 cc syringes (sterile single use). The smaller syringe slowed down the velocity of the medicine exiting the needle reducing the pain evoked by the injection.
Every knee injection was done under sterile technique. I always wore sterile, single use gloves and prepped the area with alcohol prior to the injection. When prepping we always waited until the disinfectant dried as it is only effective having dried.

I recall in my training many Doctors injecting before the skin prep had dried. I believe our habit of waiting a few extra minutes until drying occurred may be the reason why there was never an injection related infection in nearly 30 years of doing these injections.
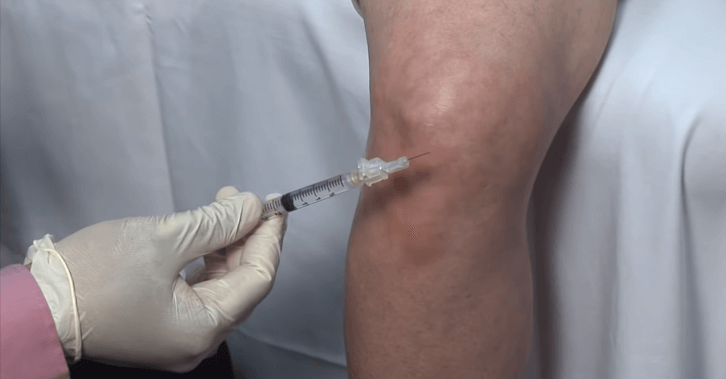
The Injection Technique
There are several approaches to the knee as to where to insert the needle. In my training I was taught to lay the patient down and, while their leg was straight at the knee, slide the needle under the knee cap (the patella) from the side to enter the interior of the knee for injection. Many patients found this rather uncomfortable as perhaps 50% of the time the Doctor finds themselves scraping the bottom of the patella as the needle is advanced.
Alternatively, I changed my approach and had the patient sit on the end of the examining table with the knee bent at 90 degrees. In this position, the patella “hugs” the knee and 2 very ample spaces open on either side of it. The needle is then passed a short distance through the skin where it immediately enters the interior of the knee without scraping any bone surfaces or cartilage.
https://www.youtube.com/watch?v=nHGsN1ZeWrI
Overall, my patients told me it was the most painless knee injection they had ever had. They would return without any pre-injection anxiety when the previous injections have been nearly painless.
Possible Side Effects of Knee Injection
As I have already stated, I cannot recall any side effects, allergic reactions, or infections that resulted from injections of the knee. Naturally, any allergic history the patient may have regarding the substances used for this procedure must be identified prior to the injection.
I would never inject an already infected knee (drainage only). Furthermore, I always avoided puncturing the skin if there was evidence of infection at the puncture site or a large varicose vein. To me these are common sense and may not even be worthy of mentioning.
Expected Results
Everyone of my patients, and I mean everyone, received significant relief from our knee injection technique. I always made sure that we had an accurate diagnosis prior to the procedure. I never injected someone with an acute knee injury.
How Often Can You Get These Injections ?
The literature on knee injections all seems to limit the number of injections to no more than 4 per year. If you examine the studies done they are fairly poorly structured. Sometimes in medicine a certain habit gets taught and ingrained into Doctors without it really being truth.
The challenge my patients had was that their pain returned several weeks after their injection. What were they to do if their next injection was 1 or 2 months away? This also prompted me to lighten the doses of each injectable (as I have already enumerated) so that I could increase the frequency of injection. I would estimate that the average patient who was on a knee injection schedule came in every 4 weeks.
WITH THE TECHNIQUE I HAVE DESCRIBED TO YOU MY PATIENTS ALWAYS RECEIVED A REDUCTION IN THEIR PAIN, THERE WERE NEVER ANY REPORTED SIDE EFFECTS, NEVER ANY REPORTED ALLERGIC REACTIONS, AND NEVER ANY INJECTION ASSOCIATED INFECTIONS. ON AVERAGE I SAW 30 PEOPLE PER DAY FOR OVER 26 YEARS…SURELY LONG ENOUGH TO OBSERVE ANY ILL EFFECTS THAT MAY HAVE OCCURRED FROM OUR PRACTICE.
Important Note
THIS MONOGRAPH IS INTENDED AS INFORMATIONAL ONLY AND NOT AS MEDICAL ADVICE. EVERY PATIENT RECEIVING A KNEE INJECTION MUST HAVE A THOROUGH HISTORY AND PHYSICAL PERFORMED BY A LICENSED MEDICAL PRACTITIONER.
Final Comments
I have carefully enumerated for you the best way to perform a knee injection (in my opinion). You now know more about the technique than most physicians do. I would recommend you find a practitioner who is willing to do the best knee injections…that is, doing it the way I have described for you.
Wishing you healing and much joy,