Polymyalgia Rheumatica and Giant Cell Arteritis
These two conditions are closely linked, and some doctors believe they are different aspects of the same disease. (Ten to 15 percent of people with polymyalgia rheumatica also have giant cell arteritis, and smilarly, 40 percent of people with giant cell arteritis have polymyalgia rheumatica.
Polymyalgia Rheumatica
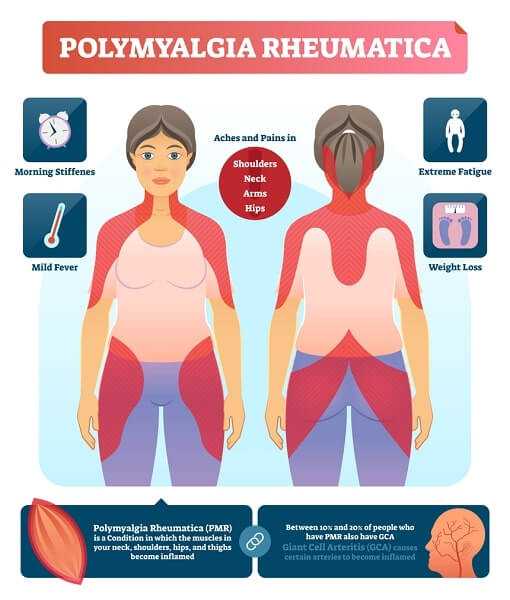
This realtively “new” disease wasn’t named until 1957, partly because it can be difficult to diagnose. But about 5 out of 1000 people have it, most of them over 50, Twice as many women as men have Polymyalgia Rheumatica, and it’s more common in White people than in people of African descent. The early symptoms are similar in many ways to those of rheumatoid arthritis: The linings of the shoulder joints (synovial tisues) are often inflamed, though the muscles are normal.
Symtomps
Morning pain and stiffness ocur in the neck, hips and shoulders, with pain felt on both sides of the body in the same places. Moving makes the muscle pain worse. You may be tired and lose weight without intending to. You may also have low fever, night sweats, and depression.
Diagnosis
Different doctors propose different methods for diagnosing polymyalgia rheumatica, as there is no single standart test. But they will take particular note if you are older than 50, have no rheumatoid factor and negative antinuclear antibodies, anda re experiencing at least three of these symtopms:
- Pain in the neck, shoulder, or hip
- Morning stiffness that lasts more than an hour
- A high sed rate, aboce 40 milimeters per hour (although about 13 percent will percent will have a normal sed rate)
- A rapid response to a dose prednisone(a corticosteroid)
Many people will have a sed rate above 100 milimeters per hour, plus mild anemia and raised platelet count. One-third of people with polymyalgia rheumatica will have slightly abnormal liver function tests. Your doctor may run these tests: sed rate, complete blood count, thyroid function, chest X-ray, rheumatoid factor, synovial fluid test, a biochemical profile and a few others.

Treatment
NSAIDs may help control symptoms for a few people with disease, but corticosteroids are almost always necessary. Treatment usually continues for one to three years, but for some people it may take longer. Unfortunately, corticosteroids can have significant and serious side effects, including infections, broken bones due to osteoporosis, and difficulty in controlling diabetes and high blood pressure. Your doctor will monitör you to help offset these problems.

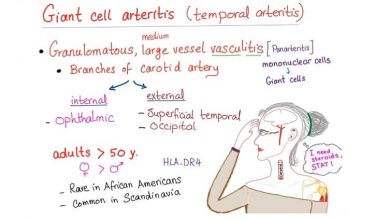
Giant Cell Arteritis
This disease, in which some blood vesesls become inflamed, has a sometimes puzzling link with polymyalgia rheumatica. In Scandinavia, nearly half the time they occur together; in the northern United States, they occur together in 320 people out of 100. Oddly, though, both diseases occur together only a tiny percentage of the time in Israel. Giant cell arteritis can appear before, during, or after polymyalgia rheumatica. As with polymyalgia rheumatica, those affected are mostly white females over the age of 50, and there’s probably a genetic link. Three times as many as men have it.
The major difference is that unlike polymyalgia rheumatica, giant cell arteritis can potentially cause blindness. Also, altough polymyalgia rheumatica responds to low-dose prednisone (10 to 20 miligrams per day), giant cell arteritis requires a higher dose of 40 to 60 milligrams daily.
Symptoms
They can be flu-like, but with no apparent virus. Symptoms include fatigue, severe headaches, diffuculty hearing, pain in the joints and tender scalp. Blurry or double vision and sometimes even loss of vision, can develop. Some sufferers will have thick, tender arteries with weak pulses. If untreated, giant cell arteritis can lead to blindness, stroke or heart attack.
Diagnosis
Test your doctor is likely to run are the same as for polymyalgia rheumatica: sed rate, complete blood count and liver function tests. Sed rate may be higher than normal. Your doctor will also probably do a temporal artery biopsy, a minor operation that involves taking a very small piece of the artery from your temple, in front of your ear and examining it under a microscope. However, inflammation in this artery doesn’t show up in 10 to 20 percent of people with this disease.

Treatment
High doses of corticosteroids are the standard treatment. Dramatic improvement is usually seen within a few days.