The Truth About Rheumatoid Arthritis Treatment

Consider This…
Nearly everyone has heard of Rheumatoid Arthritis (RA). When I was growing up, having RA was akin to being told you would be in a wheelchair soon. It was frightening. I remember working as an orderly in our local hospital and taking care of several people that were bedridden from the disease.
Then I went to medical school. It was 1978 and the field of immunology was emerging. Our understanding of RA was still limited…as were our treatments. Steroid injections were the norm in those days with limited results. Medications by mouth were mainly non-steroidal anti-inflammatories (NSAIDs).
Medications that effected the immune system had severe potential for side-effects. Even then, their effect was not generally understood or appreciated. Things were looking a little better for the RA patient but still the outcome was poor.
In the mid-1980s the AIDS epidemic swept across America. Interest in the human immune system took center stage in many research institutions as this plague was confronted. Many innocent people lost their lives before effective therapy was developed.
Ironically, the AIDS epidemic has resulted in many unexpected advances in medicine. In confronting the AIDS virus, our understanding of the intricacies of the human immune system expanded dramatically. With it came a whole new class of immune modulating medications…some of which have improved the outcome of RA patients.
This post will be a brief review on Rheumatoid Arthritis treatment. In order to understand treatment I will need to walk you through the basics of Rheumatoid Arthritis.
What is Rheumatoid Arthritis ?
RA is a systemic form of arthritis that occurs when the body “fails to recognize self” and launches an immunologic attack against itself. Normally, our immune system is responsible for patrolling our bodies and subduing invasion by any foreign substance. There are very few existing foreign substances that don’t signal our immune system to counterattack.
Each human body is distinct and part of maintaining our distinction is the “patrol and subdue” function of our immune system. Each human being has distinct markers on the surface of every cell of the body. These markers identify the owner. The only exception to this biological identification system is in identical twins.
In RA there is a misidentification which results in a systemic “auto-immune” reaction. So it is that Rheumatoid Arthritis (RA) is called an Autoimmune Disease. RA is only one of many types of these diseases. RA can effect more than the joints. Furthermore, not all arthritis is caused by this mechanism (click here to see a recent post on Osteoarthritis).
Who Gets Rheumatoid Arthritis ?
Recent census data indicates that about 1.3 million American adults have Rheumatoid Arthritis (remember this statistic does not include all forms of arthritis). There is a tendency for women to develop RA more than men. However, when men do develop it, the disease is more aggressive and more severe.
Though a human being can develop it at nearly any age, most cases occur after age 30 years and before age 65. There is a very challenging form of this disease called Juvenile Rheumatoid Arthritis that I will cover in a later post.
How Does Rheumatoid Arthritis Happen ?
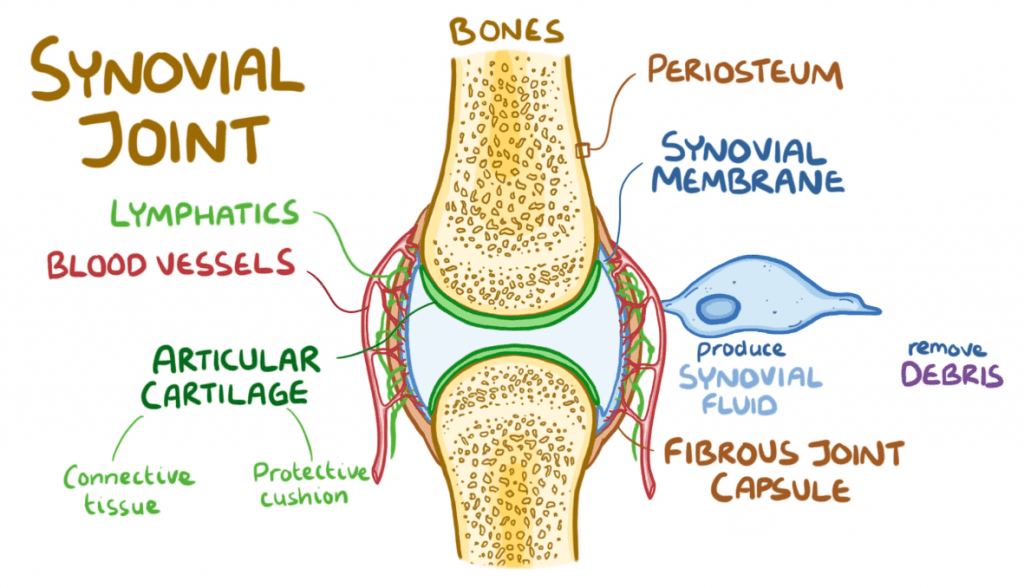
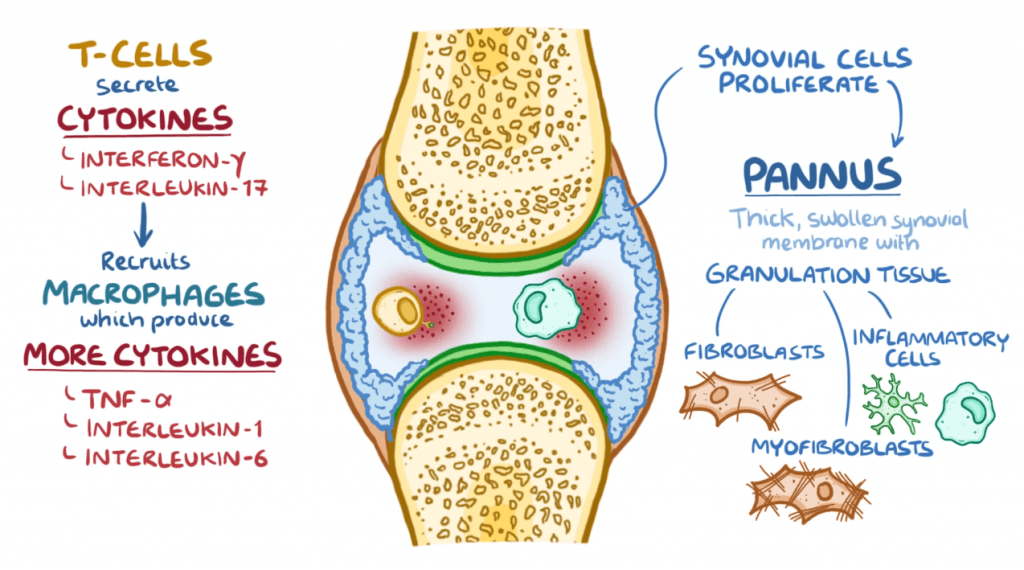
In RA, a particular area of the joint called the synovial membrane becomes the point of immune attack. As the membrane is attacked it causes the joint to swell, hurt, and fill with fluid. In most occurrences the attack subsides spontaneously leaving the joint injured.

As the attacks cycle, the joint is repeatedly injured until the cartilage, ligaments, and tendons become irreversibly effected. Eventually the bone itself is pitted and collapses. At that point the joint destruction will require replacement, fusion, or even amputation.
How is Rheumatoid Arthritis Diagnosed ?
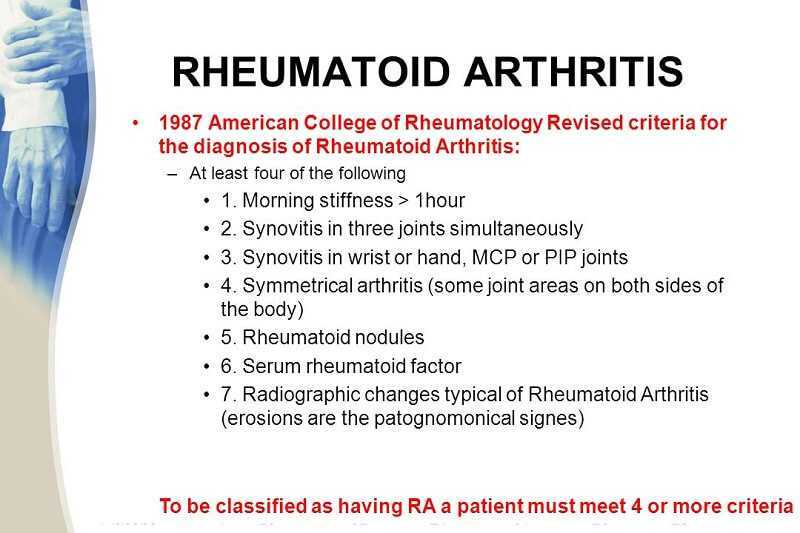
The diagnosis of RA is a combination of history, physical, and diagnostic studies:
History:
- Early morning stiffness of joints
- Symmetrical swelling of joints (both sides of the body). This is especially noted in the smaller joints (such as the hands).
- Female
- Family history of RA or other autoimmune disease
Physical:
- The presence of joint swelling in non-weight bearing as well as weight bearing joints.
- There may be nodules under the skin (often located in or near the joints effected). They can be as small as a pea or as large as a walnut.
Diagnostic Studies:
- A blood count often shows an anemia. This is non-specific for RA.
- Blood tests for inflammation are usually positive (such as an ESR or CRP). This is also non-specific for RA.
- Specialized lab tests for RA are often positive (such as CCP or RF testing). These are specific anti-body tests that are more specific for RA.
The above tests are performed by a simple tube of blood taken from the person suspected to have RA.
Additional testing for RA can also include x-rays of the involved joints. X-rays are helpful in determining how deteriorated a joint has become.
How is Rheumatoid Arthritis Treated ?
I divide the treatment of RA into 7 areas:
- Mechanical treatments:
These treatments reduce the stress on the inflamed joints involved. Resting an intensely swollen joint is essential. Mechanical stress continually applied to an inflamed joint will only worsen the joint’s deterioration.
In some cases bracing of the joint will reduce mechanical stress while still allowing for some use of the joint. This is particularly helpful with RA of the knee, wrist, neck, and back (click here to see my post on back bracing).
- Anti-inflammatory treatments:
Medications such as aspirin (still one of the best treatments for RA), Motrin, and Prednisone can be very helpful in reducing the swelling and pain of RA. There are serious potential side effects to all these medications (from life threatening gastro-intestinal hemorrhage to induction of a heart attack).
These medications do not modify the joint destruction of RA but treat the symptoms only. They can be administered through the skin (as a liquid, cream, oil, or gel) which will lower their gastro-intestinal toxicity.
- Counter-irritative treatments:
Nearly any irritation or stimulation of the skin can potentially reduce pain. In fact, some rather remote skin stimulation (from the painful joint) can reduce pain. So it is that various creams, salves, and even acupuncture actually reduce pain (click here to see my latest post on acupuncture). Capsaicin (a very irritative salve) works in this way also.
Creams are best applied directly over the swollen joint…acupuncture works through a counter-irritation of small nerve fibers called C-fibers. Because the nervous system is different from person to person (especially true for pain mediation) the effects of these modalities is unpredictable.
- Injection treatments:
My generation of physician used joint injections extensively for the treatment of RA (I did the bulk of my medical training in the 1980s). Though helpful for the reduction of pain, the effect was usually short lived and uncomfortable to administer. The insurance coverage for the injections limited their number and duration. Many doctors will use them as an adjunct with other treatments.
- DMARDS (Disease Modifying Anti-Rheumatic Drugs):
Perhaps the greatest single improvement to the treatment of RA has been the development of this class of medications. Whereas, there had been treatments that decreased pain and inflammation, earlier medications did not change the progression of the RA. Everything changed with DMARDS.
DMARDS not only will reduce pain and inflammation but, the previous unrelenting progression to joint destruction has been largely stopped by this class of medication. Most types can be taken by mouth. They require the careful administration by a health care practitioner familiar with the idiosyncrasies of this class of medication.
The most common side effect of this type of medication is a reduction in immune reactivity to the point that a simple infection could be lethal. Furthermore, the induction of immune related cancers is a devastating complication of these medications.
- Surgical treatments:
There is a subgroup of people with RA that respond poorly to therapy or did not have access to therapy. They will subsequently have joint destruction that will require replacement. Replacement of a joint will remove the synovial membrane and halt the inflammation in that joint. However, other joints still remain at risk (multiple joint replacements is not uncommon in RA).
- Pain modifying medications:
Finally, despite the best efforts of all involved, simple treatment of the pain may be all that can be done. Under such circumstances the dose of opiate pain medications may be quite large. It is the compassionate thing to do for a patient with extensive RA, in my opinion.
Final Comments
I have briefly reviewed RA for you. I hope you have enjoyed this post. Don’t forget to send me a comment or question below.
I wish you much joy and good health,
A BRIEF VIDEO REVIEW OF THIS POST: