Sciatic Nerve Treatment Options

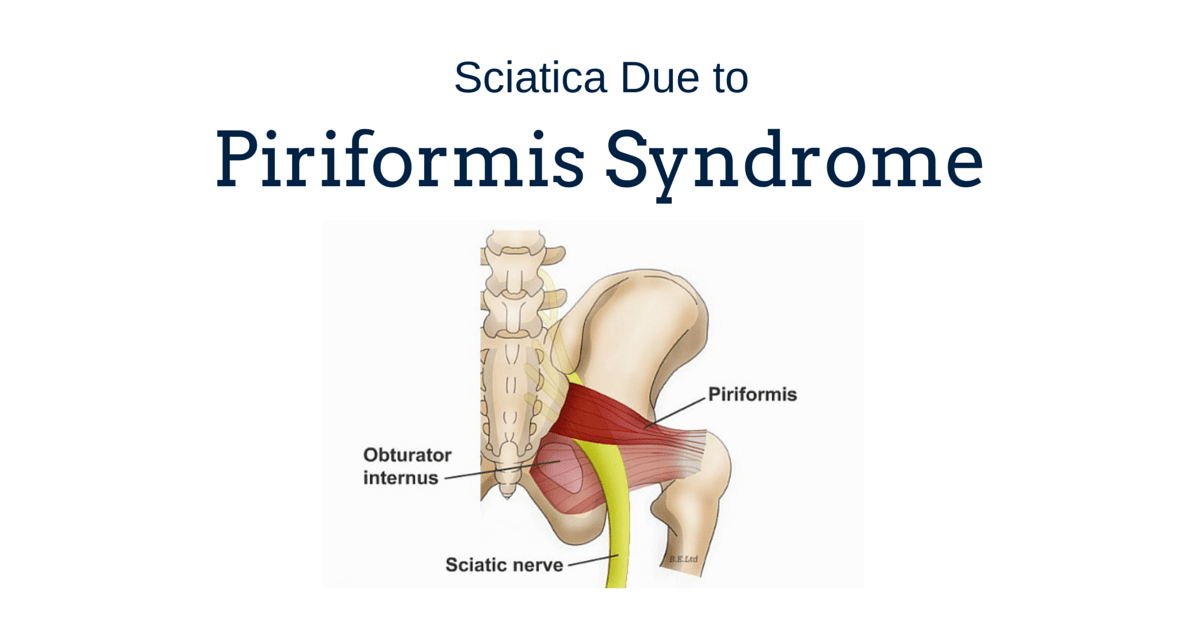
Sciatica or sciatic nerve pain can be an extremely debilitating symptom, with sufferers experiencing both acute and chronic pain in the buttock and back of the thigh. This can be a sharp pain or a dull ache and is often relieved when bending forward, lying down, or when riding a bike, but is exacerbated by walking, bending backwards, and twisting the spine. The exact cause of the sciatica can often be pinpointed through a thorough physical examination and accurate description of symptoms to the diagnosing physician. If the pain originates in the thigh, just above the knee then it is likely due to the piriformis muscle that provides lateral thigh movement, rather than the spine itself. If the pain is below the knee and into the foot, and there are poor reflexes or a decreased ability to raise the foot then the sciatic nerve may be being pinched at the L3-L4 level.
Pain in the side of the foot and the ankle, with poor ankle reflexes and difficulty in lifting the heal indicates a potential nerve impingement at L5-S1 in the lower lumbar spine. Foot-drop, often associated with conditions such as Multiple Sclerosis, can also be suggestive of pinched nerve at L4-L5, especially where the big toe is particularly painful and there is pain or numbness along the up of the foot. It is important for patients to accurately express their symptoms in order to facilitate a speedy diagnosis and access appropriate treatment. Sciatica can describe a number of painful and uncomfortable experiences due to a pinched nerve and in some cases sciatic nerve treatment may be through back surgery at that level of the spine.

Conservative sciatic nerve treatment is usually offered for six months prior to any surgery and this can often relieve the sciatica symptoms to a manageable degree. Physical therapy, medications such as NSAIDs, and supportive devices to restrict backwards bending are frequently utilized with varying degrees of success. If, however, the symptoms become intense and incapacitating, significant weakness occurs in the legs, or if bowel or bladder incontinence develops, surgery is usually scheduled quite quickly in order to prevent possible permanent nerve damage. Spinal stenosis causing sciatica can be addressed through various surgical procedures depending on the extent of the problem. If compression is indicated at a single level then a microendoscopic procedure may be possible, whereas larger problems ranging over a number of vertebrae will require more radical and invasive approaches. Back Surgery may simply prevent the condition from getting any worse, rather than relieving the pain and patients should discuss their expectations with their physician regarding sciatic nerve treatment through surgery.
Minimally Invasive Surgery for Sciatica
Microsurgery as a sciatic nerve treatment can take the form of microdiscectomy, microlaminoforaminotomy, microlaminotomy, X-Stop, and TLIF, amongst other procedures. Minimally invasive back surgery involves the use of a series of dilators of increasing size to reach the deeper tissues of the back through a much smaller incision than in the traditional open procedure. The surgeon will make use of an endoscope (a tube with a camera on the end) to visualise the area they are operating on. Small, specialized, surgical instruments will also be fed through the tubular retractor to be used by the surgeon when cutting away the material compressing the spinal nerves, and extracting the herniated disc material. Microdiscectomy has a shorter procedure time (around 45mins) compared to open discectomy (73mins), and usually leads to a faster recovery by the patient with less complications. Around 90% to 95% of patients experience relief from sciatica after undergoing a microdiscectomy. In some cases an open procedure may still be necessary, such as when other forms of compression such a ligament calcification or osteophyte growth are present or when spinal fusion needs to occur in conjunction with the discectomy.
Discectomy for Sciatica
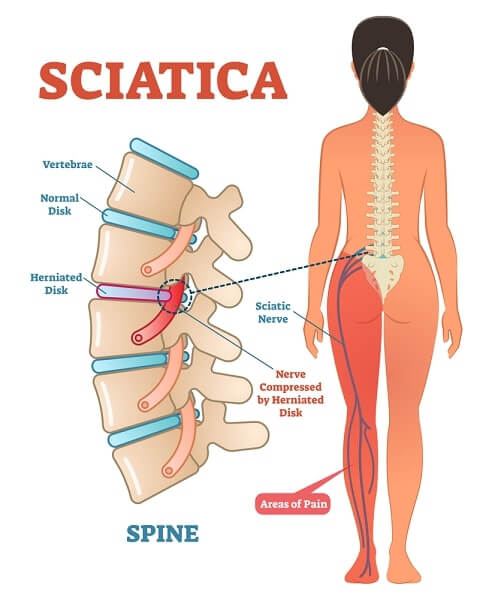
The symptoms of sciatica are largely due to the compression of nerves and blood vessels in and around the spine by the bulging matter of the intervertebral disc, the presence of osteophytes (bone spurs), calcified tissue, or spinal instability and curvature. In a spinal treatment to address sciatica it is important that the material causing the compression is removed and the spine is stabilized so as to reduce the risk of further stenosis occurring. A discectomy for sciatica is the excision of a fragment of herniated or bulging disc material or the whole of a disc that has degenerated and herniated which was pressing on a nerve. This can decompress the lumbar spine and allow the nerves to begin healing, where possible. Compression at L2-S1 may cause sciatica symptoms and a number of levels may require the removal of material pinching the nerves.
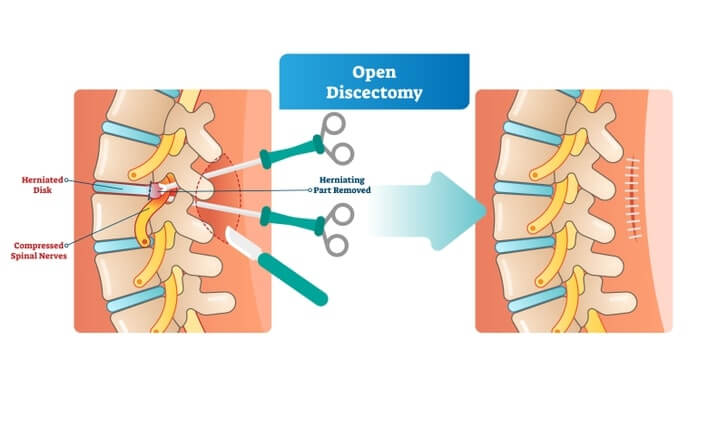
Traditional open discectomy is a back surgery that involves the surgeon making an incision in the back, just above the problematic disc, and the moving aside of the muscles, nerves, and ligaments to gain access to the herniation and remove the disc or disc fragments. It is often necessary in this open procedure to sever some muscle and ligaments to gain access to the disc. A microsurgery technique may be available depending on the location of the disc bulge or herniation and is, in most cases, preferable to the traditional open technique. Most surgeons will use a posterior approach for the removal of bulging or herniated disc material in the lumbar spine as the compression usually occurs at the back of the spine. An anterior approach may be used for disc herniation in the neck but is rare in a discectomy for sciatica.
Microlaminoforaminotomy for Sciatica
Microlaminoforaminotomy is a keyhole spine surgical procedure conducted from the posterior spine to treat lateral disc herniation. By using this technique, surgeons can retain the mobility of the section of vertebrae treated and minimize trauma to the muscles and ligaments of the lumbar spine. The surgeon is also able to remove just a portion of the herniated disc, thereby maintaining some degree of cushioning between the vertebrae and reducing the patient’s risk of losing intervertebral height and suffering spinal curvature. This type of back surgery is often considered where patients are suffering from radicular pain, paraesthesias, sciatica pain, problems with motor skills, and loss of sensation, or numbness, due to disc bulging, or herniation, osteophyte growth, or ligament calcification and compression.
Operations are performed at a single level, and make use of specialized surgical instruments such as the burr to cut away a tiny portion of the lamina (often only around 3mm) and remove the compression material through this hole. Most patients do not require a second surgery to correct spinal instability which may occur if a larger portion of the lamina is removed. Recovery is often very short, with patients leaving hospital within the day and able to return to work relatively quickly.
Foraminotomy for Sciatica
A foraminotomy for sciatica is another spine surgery option which may be preferable for patients who show evidence of significant obstructive tissue or bone in the spinal canal. If there is a large area of osteophyte growth narrowing the foramen then a traditional open procedure may be more effective in removing this material than the minimal access surgery where it can be difficult to extract larger tissue bodies. A foraminotomy aims to widen the spaces through which the lumbar nerves exit the spine thereby removing the compression which is responsible for sciatica symptoms. Abnormal bone growth, thickened ligaments, or even a portion of bone from the vertebrae themselves may require removal to relieve patients’ symptoms of radicular pain, weakness, numbness, paraesthesia, and tingling in the lower back and down the legs into the feet.
The success rate for foraminotomy is relatively high compared to many other back surgeries. The minimally invasive surgical techniques, such as microlaminoforaminotomy, can reduce risks and improve the prognosis even further. Sometimes a surgeon may perform a discectomy after the foraminotomy if there is evidence of significant disc degeneration. The disc may be palpated if it is bulging so as to encourage decompression and proper reconfiguration of the vertebral space. Fusion is not normally necessary with a foraminotomy as only small amounts of structural material are removed. The surgeon may use a burr to shave the edge off the inside of the facet joint and possibly a small portion of the ring at the back of the vertebrae above or below the site of nerve compression. If more than one level of vertebrae is being operated on then the surgeon will either use the existing incision prior to closing the overlying skin back together, or make a separate incision at the appropriate level.
Laminectomy for Sciatica
Laminectomy, laminoplasty, and laminotomy may all relieve the pressure on lumbar nerves which is causing sciatica. The more extensive the removal of structural tissue, the more likely a patient is to require additional spinal fusion surgery, with microsurgery preferable for patients with fairly straightforward spinal stenosis in the lumbar spine. If significant canal stenosis is present at numerous levels then a laminotomy or small scale laminoplasty is unlikely to provide as extensive relief from sciatica as a laminectomy with fusion.

A laminotomy may be performed to provide the surgeon access to bulging or herniated disc material, or osteophytes, and can be carried out using minimally invasive surgical techniques. The laminotomy procedure leaves the majority of the back bone to stabilize the spine, unlike a laminectomy, and may be preferred in cases where stenosis exists at only one level as indicated by fairly specific sciatica symptoms. Laminoplasty is a type of back surgery where the laminae is scored on one side and opened like a door, with metal plates attached in order to maintain this position. The extra space allows the spinal canal to relax and relieves pressure on the spinal nerves and cord. Laminoplasty has the advantage of creating a reasonable amount of space for decompression purposes whilst maintaining the structure of the spine and reducing the need for fusion due to instability. Laminoplasty may be helpful for patients with spinal stenosis causing sciatica at one or more levels in the lumbar spine but may be dismissed in favor of a laminectomy with fusion if the patient exhibits signs of spinal instability or other complication.
Laminectomy with or without Fusion
Sciatica which involves stenosis at a number of intervertebral levels may be treated using a combination of a laminectomy, followed by a discectomy, or partial discectomy followed by a spinal fusion procedure. The laminectomy removes a portion of the back bone and can grant the surgeon excellent access to the material which is compressing the spinal nerves. This may be a bulging or herniated disc, fragments of bone or disc that have worked themselves loose, osteophyte growth, or calcified ligaments in the exterior spine putting pressure on the nerves as they exit the spine. Spondylolisthesis is another possible cause of sciatica, with the slightly offset vertebrae causing nerve compression. Back surgery to correct spondylolisthesis and stabilize the lumbar spine is likely to provide the most relief and will usually involve spinal fusion.
After the offending material has been removed the surgeon may perform spinal fusion in order to maintain, or restore, the intervertebral height at that section and reduce the risk of segmental motion. Discectomy, laminectomy, and fusion are more likely in cases where considerably osteophyte growth exists across a number of vertebral levels, or where multiple herniation and bulging is observed across a number of levels. Fusion may be in the form of an autograft, with bone taken from the patient’s hip and secured by rods and screws, or an allograft, where donor bone is utilized. Laminectomy is a major back surgery and requires the cutting of muscle and ligaments to reach the back bone.
There are possible complications surrounding the extent of structural tissue removed and its resulting effect on the stability of the spine. Patients need to be cautious about twisting and bending the spine during their recovery in order to prevent hardware failure or graft movement. The rigidity after spinal fusion can cause pressure to be deferred onto the adjacent segments and lead to fracture or other problems at those levels. Recovery from laminectomy can be prolonged and surgeons favour more minor procedures where they will be as helpful. Patients are usually advised against using NSAIDs after a fusion procedure as this can affect the formation of a solid union. Smoking is a major risk factor for pseudoarthrosis, with some surgeons unwilling to operate on those who have failed to quite smoking prior to the back surgery. Around 70-80% of patients with sciatica who undergo a lumbar laminectomy experience some degree of relief from their symptoms.