Sex And Chronic Pain

Could It Get Any Worse?
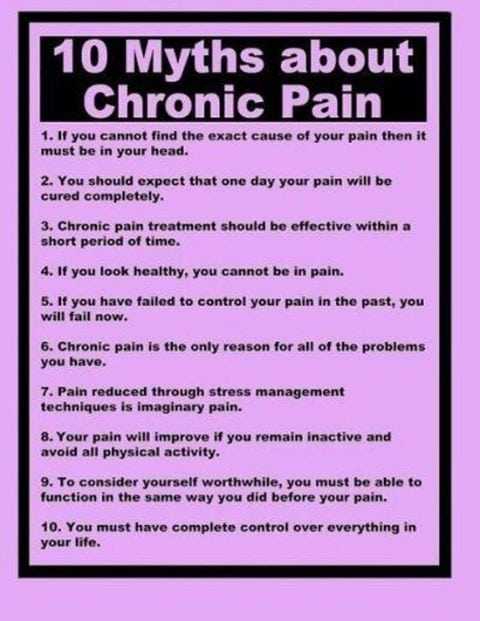
Joseph shuffled into the office with a frown on his face. “Doc, I am in so much pain. Every minute of everyday I have to deal with this pain in my abdomen. My surgeon thought it was my Gallbladder so he took it out…my pain continued.”

“My Internist thought I had some type of psychiatric cause for my pain…so he referred me to a Psychiatrist who medicated me so heavily that I was falling asleep driving my car…I still hurt. And Doc…with all the pain…I haven’t made love to my wife in 6 years. Could it get any worse for me?”
Since chronic pain touches every aspect of a person’s life, sexual dysfunction in a person with chronic pain should be no surprise. National statistics on sexual dysfunction in the United States ranges from 30-40 percent…in people without chronic pain.
I have never been a fan of sexual statistics. It’s one of those topics that people have a hard time being totally honest about. In my clinical practice of pain management nearly every chronic pain patient had some type of problem with sexual intimacy…if I was willing to listen and they were willing to tell me.
Why Is There Sexual Dysfunction With Chronic Pain?
The physiologic response in human sexuality is complicated. Human beings are complicated enough without having chronic pain and chronic pain medications and the emotional response to chronic pain, and…etc., etc., etc.. The human body does not compartmentalize each organ system…the way it is taught in medical school.
There are 3 basic mechanisms to disrupt human sexual function in people with chronic pain:
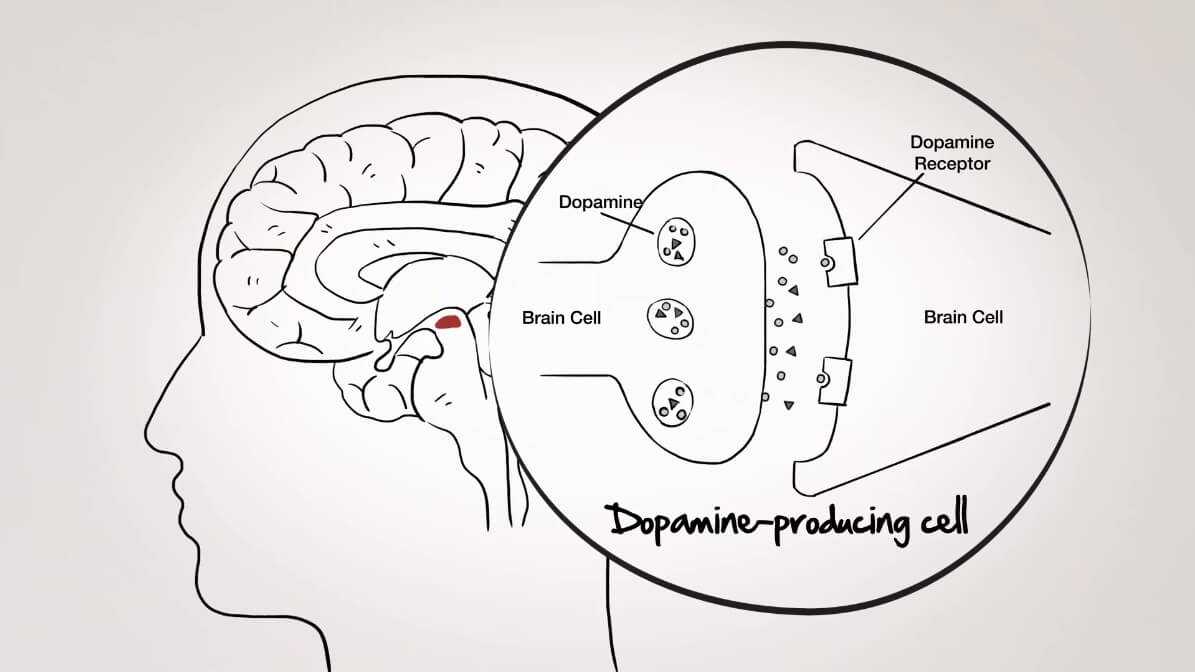
- The most obvious is the very neurochemistry of pain. Intractable pain raises cortisol , reduces dopamine, reduces serotonin, reduces norepinephrine, and reduces oxytocin. Normal levels of these neurotransmitters are essential to a “normal” sexual response.
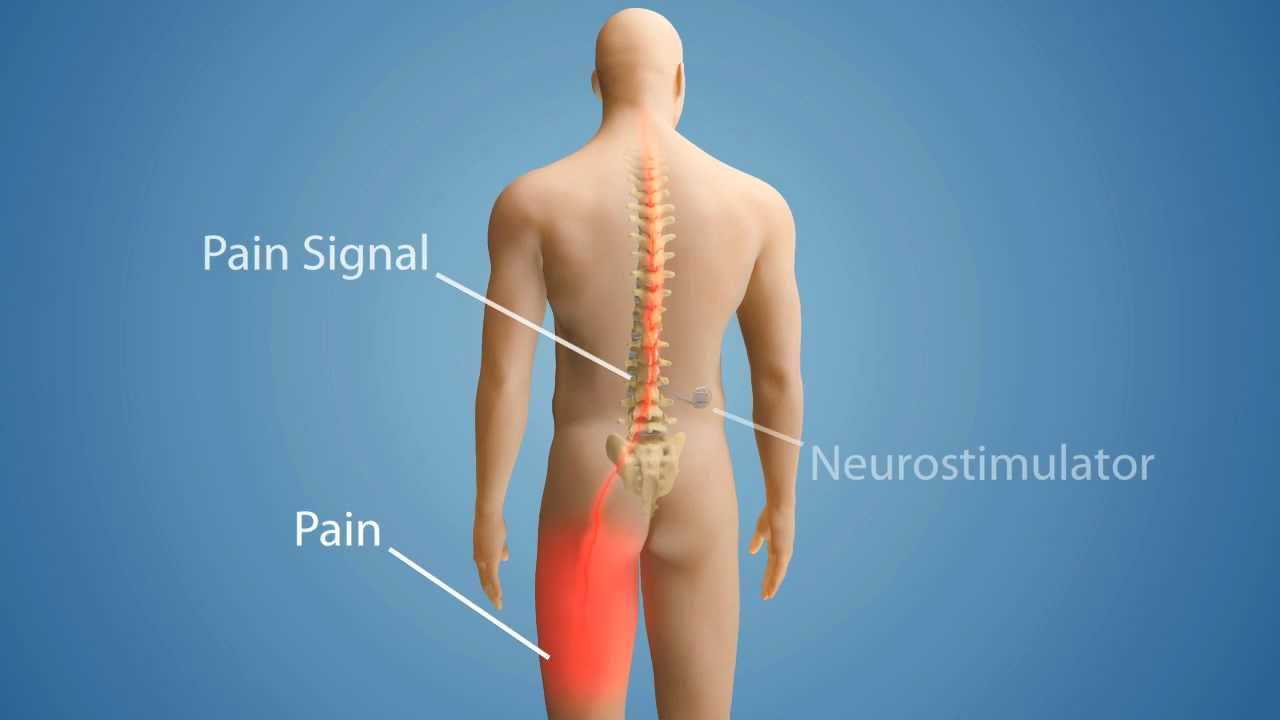
- The nature of the mechanism causing the pain. Some chronic pain syndromes effect the very mechanics for human sexual response (ie. chronic lumbar pain). Other chronic pain syndromes are directly related to intercourse and “torpedo” the intimacy (ie. chronic pelvic pain).
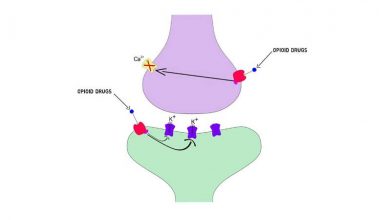
- The treatments for chronic pain can profoundly effect the human sexual response. Opiate pain medications lower testosterone levels when taken long term. Certain surgeries can disrupt pelvic nerves literally disconnecting the sexual neural circuits.
Like I said before, “it’s complicated.” When a person has to endure chronic pain their sexual intimacy will ALWAYS be effected somehow. If depression is the “first cousin” of chronic pain, sexual dysfunction has to be the “brother or sister” to it.
What Can I Do To Normalize My Sexual Function?
Thankfully, there are several important measures that can be taken to restore sexual intimacy in a person with chronic pain:
- First, and foremost, effectively treat the pain. The likelihood that people with chronic pain will achieve a totally pain free state is uncommon. However, predictable pain relief to a tolerable level (most people would report a “5” as tolerable) does wonders for a person’s sexual response.
- Understand the mechanism for the pain generation and devise a strategy to counteract it’s effect on the sexual response. For instance, if the person suffers from chronic hip pain, body positioning during sexual intercouse can reduce pain significantly. Discussions of this type are very private and require time with your pain practitioner.
- Identify the reversible sexual side effects of the treatments. I used to run all the medications I was treating a person with through a side effect program that I kept on my i-phone (very handy in clinical practice).
There Is Hope…
Joseph’s pain was treated with a “high tech” mechanism. I had a surgeon implant a long term intravenous line into a large vein underneath his collar bone. Through it I infused a continuous pain medicine called Nubain.

We were able to wean him off all of his other pain medications. The infusion was powered by an external battery powered pump (it was carried in a small “fanny pack” which he wore continuously). Myself or a home visiting IV Therapy nurse could adjust the dose of the Nubain by adjusting the pump rate.
His pain was well controlled and he had no side effects from the low dose Nubain. When he returned to my office for his first post-hospitalization visit he was smiling. He said, ” I made love to my wife for the first time in 6 years. You are the best, Doc”…I was reminded why I had gone into medicine.
If you would like to leave a comment or question please do so below. I would love to be of service to you.
Wishing you joy and healing,