Special Remedies for Special Symptoms

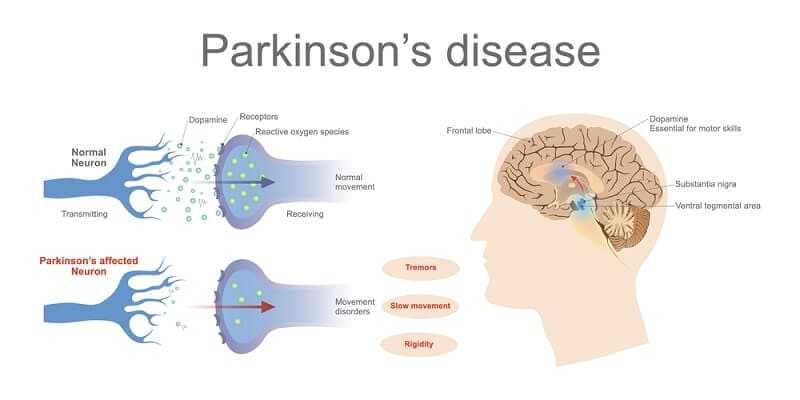
In the preceding aritcles I described the major anti-Parkinson drugs: the anticholinergics, levodopa, the dopamine receptor agonists, and amantadine. These drugs act on the parkinsonian state as a whole and are not directed specifically against any one symptom. In general, they relieve all or at least most symptoms related to the classic triad: tremor, rigidity, and bradykinesia. There remains a miscellaneous group of drugs whose acquaintance many patients are apt to make sooner or later. They are not specific for parkinsonian symptoms but rather are used to treat symptoms which are very common, such as insomnia, anxiety, constipation, etc. Some discussion of these drugs seems appropriate because Parkinson patients may react differently to these commonly used agents, and some of these drugs may interact adversely with the major anti-Parkinson drugs.
PROPRANOLOL
The drug propranolol (Inderal) is used mainly to treat irregularity of the pulse and, to a lesser extent, to control high blood pressure. It may be used for these purposes in Parkinson patients with heart disease, irregular heart rate, or high blood pressure. It may also be used to protect the heart from the possibility of levodopa causing palpitations or episodes of abnormal heart rhythm in patients who are subject to palpitations.
Propranolol, however, has also been used occasionally because it seems to have a favorable effect on tremor, at least in some patients. Because the drug has an important action on the heart, it must be used with care. It is not recommended for asthmatics or in patients who have had heart failure since it may exacerbate these conditions.
A very occasional patient who still has some disturbing tremor despite good effects on other symptoms of Parkinson’s disease may enjoy a good response to this drug. Unfortunately, propranolol has no effect on other symptoms.
Propranolol is commonly used to treat the symptom of tremor in the condition known as “benign essential tremor” or “familial tremor.” This is sometimes confused with parkinsonian because the tremor often bears a superficial resemblance. Persons with essential or familial tremor do not develop any of the other manifestations of Parkinson’s disease, however, even after 40 to 50 years. On closer examination, their tremor differs in a number of respects from that of Parkinson’s disease. One of these differences is that the tremor commonly involves the head and the voice; this rarely if ever occurs in Parkinson’s disease. Another feature is that essential tremor usually runs in families; in nearly all instances, one parent also had the condition. Finally, essential tremor responds differently to various drugs. In particular, it can be suppressed for a few hours by alcohol. The tremor of Parkinson’s disease is not reduced by alcohol. A highball or a glass of sherry dramatically diminishes the former for a few hours but not the latter. The various minor tranquilizers may also effectively reduce essential tremor, paralleling the action of alcohol. Levodopa has no effect on essential tremor but, as we noted, can greatly reduce or abolish the tremor of Parkinson’s disease.
Several new drugs, closely related to propranolol, are available. One of these, metoprolol (Lopressor), is used primarily in treating high blood pressure. It is not as effective as propranolol against tremor, but has much less risk of exacerbating asthma.
MINOR TRANQUILIZERS AND HYPNOTICS
Minor tranquilizers are sometimes prescribed for patients with tremor persisting despite treatment with the usual anti-Parkinson drugs and to relieve the sense of inner restlessness and nervousness which may occur as a symptom of Parkinson’s disease or as a side effect of the anti-Parkinson drugs. Those most commonly used are lorazapam (Ativan), diazepam (Valium), oxazepam (Serax) and alprazolam (Xanax). These drugs are called minor tranquilizers to distinguish them from the major tranquilizers, such as chlorprom-azine (Thorazine), trifluoperazine (Stelazine), and haloperidol (Haldol), which are used primarily in psychiatric practice to treat severe mental illness. The major tranquilizers, as we noted earlier, block the action of dopamine in the brain and consequently can cause parkinsonism. They therefore should not normally be given to Parkinson patients. The minor tranquilizers are entirely different and do not cause parkinsonism. They may, in fact, be quite useful but should be used sparingly and only as needed.

The minor tranquilizers can cause drowsiness, incoordination, dizziness, and confusion, and occasionally seem to increase the bradykinesia or slowness of movement of Parkinson’s disease. Moreover, some persons may become psychologically dependent on or habituated to these drugs. Patients who use these drugs heavily for a period of time and then suddenly stop taking them may suffer withdrawal symptoms, including nervousness, agitation, and even (rarely) convulsions. However, I have never encountered a Parkinson patient who became dependent on these drugs, perhaps because I am careful to prescribe them sparingly.

What can the Parkinson patient with insomnia take to induce sleep? Preferably, of course, nothing. If levodopa (whether used alone or as Sinemet) seems to be responsible for insomnia, the bedtime dose should be avoided; if the drug is necessary, it might be reduced 50%. Several old nonmedical tricks may be quite helpful in inducing sleep at night, including a warm drink (such as a glass of warm milk) or even a brandy at bedtime. If insomnia is still a problem, a mild sedative such as chloral hydrate may be used. This is a very old and mild short-acting sedative that leaves no hangover and is least apt of all the available hypnotics to cause confusion. It is made in the form of 0.25- and 0.5-gram capsules. Your physician may direct you to take one capsule on retiring and if necessary to take another capsule an hour later. Two capsules (1.0 gram) may be used on retiring if one is not effective. A mild tranquilizer such as lorazepam (Ativan) 1 mg at bedtime may also be helpful.

Parkinson patients more commonly have no trouble falling asleep on initially retiring. Rather, their problem is that they wake up after several hours and then cannot get to sleep again. If there are recurrent Parkinson symptoms at that time—stiffness, cramps or just slowness—and the patient cannot fmd a comfortable position, then an additional dose of Sinemet or Madopar may be helpful.

The drugs flurazepam (Dalmane) and temazepam (Restoril) are commonly prescribed hypnotics. They are closely related to diazepam (Valium) and may also increase the bradykinesia of parkinsonism. Thus I generally avoid this drug in treating my patients.
OVER-THE-COUNTER SEDATIVES
Parkinson patients should avoid over-the-counter sedatives such as Compoz, Sominex, Sleep-eze, Nytol, and others. These preparations all contain scopolamine (hyoscine) in quantities comparable to those formerly employed in treating parkinsonism as one of the active ingredients. They also contain an over-the-counter antihistamine, metha-pyrilene hydrochloride, which like other antihistamines also has some anticholinergic activity. The addition of these agents to a Parkinson patient’s existing drug regimen, which may already include some anticholinergic agents, may carry the patient over the threshold of anticholinergic toxicity. Consequently Parkinson patients are less able to tolerate the side effects commonly produced by these medications. On the other hand, the anticholinergic properties of these formulations may have some beneficial effect on the symptoms of parkinsonism. Patients should consult their doctors before trying them, however, to minimize the chance of an unpleasant interaction with their own anti-Parkinson drug treatment.
DIURETICS
Swelling of the feet due to the accumulation of water in the tissues (edema) of the legs and feet is a common manifestation of parkinsonism. It is often more marked in one leg, nearly always the leg on the side where the first symptoms occurred. The causes of this swelling are not fully understood. One reason may be that there is less muscular activity in that limb due to the bradykinesia of parkinsonism. In any event, the swelling can be relieved by diuretic agents (that is, drugs which increase the volume of urine passed in a day). Milder diuretics such as hydrochlorothiazide (Hydrodiuril) may effectively relieve this swelling. Usually only one dose once or twice a week is necessary. The drug should be taken only with a doctor’s prescription.

If the swelling was induced by the drug amantadine (Symmetrel), it should subside when that drug is stopped although it may require several weeks to disappear. If varicose veins are present, elastic hose may be helpful. Further treatment may be advised by the doctor.
LAXATIVES
Chronic constipation is a familiar symptom of Parkinson’s disease. It results from a general slowing of the muscular action of the bowel or of muscular action in other organs. As mentioned earlier, constipation is also often exacerbated by the drugs used in treating parkinsonism. The tendency of Parkinson patients to drink little water is a further complicating factor. Consequently many patients need to take laxatives.
I urge patients to try natural means of maintaining normal bowel habits. This means making an effort to drink more water, to eat adequate roughage and high-fiber foods, and to ingest prunes, prune juice, or figs regularly. Failing all this, one must resort to laxatives. Several classes of laxatives need be considered.
First, there are bulk laxatives which work by retaining water in the stools. Patients who pass small, hard stools—really dehydrated stools—may benefit from this measure alone. A common laxative in this class is Metamucil, available over the counter. A tablespoon-ful stirred in one glass of water a day may suffice.

Another useful preparation is the fecal softener dioctyl sodium sulfosuccinate. A great many proprietary over-the-counter preparation containing this ingredient are available.
One capsule one, two, or three times daily may be used. Generally, these are used on a regular daily maintenance basis by Parkinson patients.
If these measures are inadequate, the “irritant” laxatives which stimulate the bowel directly may be required. Milder ones such as bisacodyl (Dulcolax) are preferable. Some preparations combine such a stimulant with the fecal softeners mentioned above. The pharmacist can give advice about a suitable one, or the patient can check the label on the packages on the supermarket shelf, looking for the two ingredients dioctyl sodium sulfosuccinate and bisacodyl. Finally, many patients have a laxative habit acquired long before Parkinson’s disease developed. They may prefer to continue using their old favorites. As a last resort, enemas may be required to maintain adequate evacuation.
ARTIFICIAL TEARS
The reduced frequency of spontaneous eye blink which is common in parkinsonism may result in some redness and dryness of the eyes and eyelids. The lids may become encrusted. Patients feel some irritation, a dry, burning feeling in the eyes. Usually the major anti-Parkinson drugs restore eye blink to more normal frequency; with improvement in the normal “windshield wiper” function of the eyelids, these symptoms are relieved. However, if there is still some eye discomfort, irrigating the eyes with artificial tear solutions may be helpful. Various preparations of artificial tears can be purchased at local drug stores over the counter. They reproduce the salt concentration of natural tears. If symptoms are not relieved by this simple measure, medical advice should be sought.
TREATMENT FOR SEBORRHEA
The increased activity of the sebaceous gland of the skin in parkinsonism commonly results in a somewhat greasy appearance of the face and forehead (seborrhea) and occasionally in some irritation and inflammation of the skin (seborrheic dermatitis). The seborrhea and the secondary dermatitis are reduced by treatment, especially by levodopa, and are rarely serious problems. Seborrhea can be controlled by washing daily with bland or neutral soaps. A commonly used soap formulation is the acne aid bar available at most drug stores. Dermatitis responds to a variety of lotions containing small amounts of hydrocortisone or related agents, but these require a doctor’s prescription.

A variety of hair lotions are available over the counter that may satisfactorily control excessive dandruff. One of the more effective contains selenium and is marketed under the name Selsun. A more concentrated solution of selenium is also available with a doctor’s prescription. Many authorities advise that selenium preparations be used sparingly because they may cause hair loss if used excessively. It would be preferable to reserve them for a last resort and then use them only occasionally.
DRUGS FOR LEG CRAMPS
Foot and leg cramps are most often due to wearing off of the levodopa benefit. Typically, they occur early in the morning. Associated with spasm of the muscles of the calf and sole of the foot, in-turning of the foot, and clawing of the toes it represents “end-of-dose” dystonia. Measures to counteract motor fluctuations generally alleviate or prevent these cramps. These include additional doses of Sinemet or Madopar, selegiline, or a dopamine receptor agonist (Parlodel or pergolide). Failing these, one may try lioresal (Baclofen). The recommended dose is 10 mg three times daily. Double this amount, however, may be needed to yield substantial relief. Some individuals, however, have difficulty tolerating these doses of lioresal owing to nausea, dizziness, and drowsiness. Vitamin E (alphatocopherol) has been recommended by some physicians to prevent nocturnal cramps, but it has not been effective in my patients.