Spinal Cord Stimulation Trials Fail to Convince Patients

Spinal cord stimulators offer an effective treatment for intractable neuropathic pain without invasive surgery or where back surgery has failed to relieve symptoms. However, anyone with persistent neuropathic pain who is considering a spinal cord stimulation implant has to first be assessed to see if the therapy is likely to work for them.
This involves a trial that needs to demonstrate at least a 50% improvement in pain or a 50% reduction in the patient’s use of pain-relief medications, in addition to improvement in function.
In a new review the high conversion rate for spinal cord stimulation trial to implant placement has dropped dramatically. In earlier research it was found that some 63-91% of those trying out the stimulation devices went on to have spinal cord stimulators implanted in the spine. This new US national survey found that just 41.4% of patients ended up having permanent spinal cord stimulation.

Insurance companies have been much more focused in recent years on limiting coverage so that a patient can only have a single trial of a spinal cord stimulator for each specific area of their anatomy. This is in addition to questioning coverage where a specific health care provider’s conversion from trial to implant is less than half of all patients.
Regional Variation in Spinal Cord Stimulation Conversion
This may actually be good news for patients as the research has found significant variation across different areas of the US, suggesting variation in practice and assessment when dealing with spinal cord stimulation for intractatble neuropathic pain. Rates of conversion are much higher in North-Central and South regions compared to the Northeast or West.
The findings were presented by lead author Gustavo Chagoya, a medical student at Duke University in Durham, North Carolina, at the American Association of Neurological Surgeons (AANS) 82nd Annual Meeting (Abstract 816. Presented April 9, 2014). It is hoped that by looking more closely at the factors involved in conversion rates this can help demarcate those patients for whom spinal cord stimulation is likely to be of benefit.
For example, earlier research has led physicians to consider those with multiple pathologies less likely to demonstrate benefits from this treatment and to end up not having permanent implantation of the device. The new research points out that this attitude is based on studies from single institutions however, meaning that it may not be accurate for all patients across all regions.
Chagoya and colleagues looked at trials and billing data for 170 million patients in the US from 2000 to 2009. Those included had percutaneous implantation of neurostimulation electrode array (Current Procedural Terminology [CPT] code: 63650) without simultaneous implantation of a permanent pulse generator (CPT: 63685). These patients were most likely to have radculitis and/or neuritis, or postlaminectomy syndrome (a complication arising after back surgery involving removal of a large portion of the cartilagenous backbone, the lamina).
Factors Affecting Spinal Cord Stimulation Success
A range of factors were included in the analysis, such as the patients age, sex, insurance status, employment status, geographic location, number of previous percutaneous trial attempts, and primary diagnosis.
Some 21,672 patients had percutaneous trials to assess the potential for permanent spinal cord stimulation implant to relieve their symptoms. Conversion was classed as the patients receiving the implant within three months of the trial, which amounted to 8982 patients (41.4%). Age was a significant factor in conversion with only 38.3% of those over 65 progressing to the permanent implant. Younger patients had a 42% conversion rate. There was no significant difference in terms of the patients’ sex but there was a significant difference between those who had commercial insurance and those without: 43% vs. 36.8%.
Supporting the practice of health insurers, just 29% of those who had previously had a percutaneous trial for neuropathic pain converted to the permanent implant, and just 14% of those with two or more trials, compared to 44% of those with no history of such a trial.
What is Spinal Cord Stimulation?
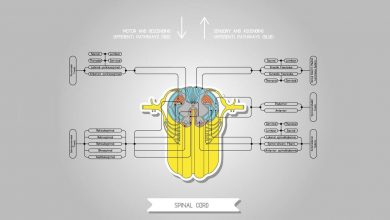
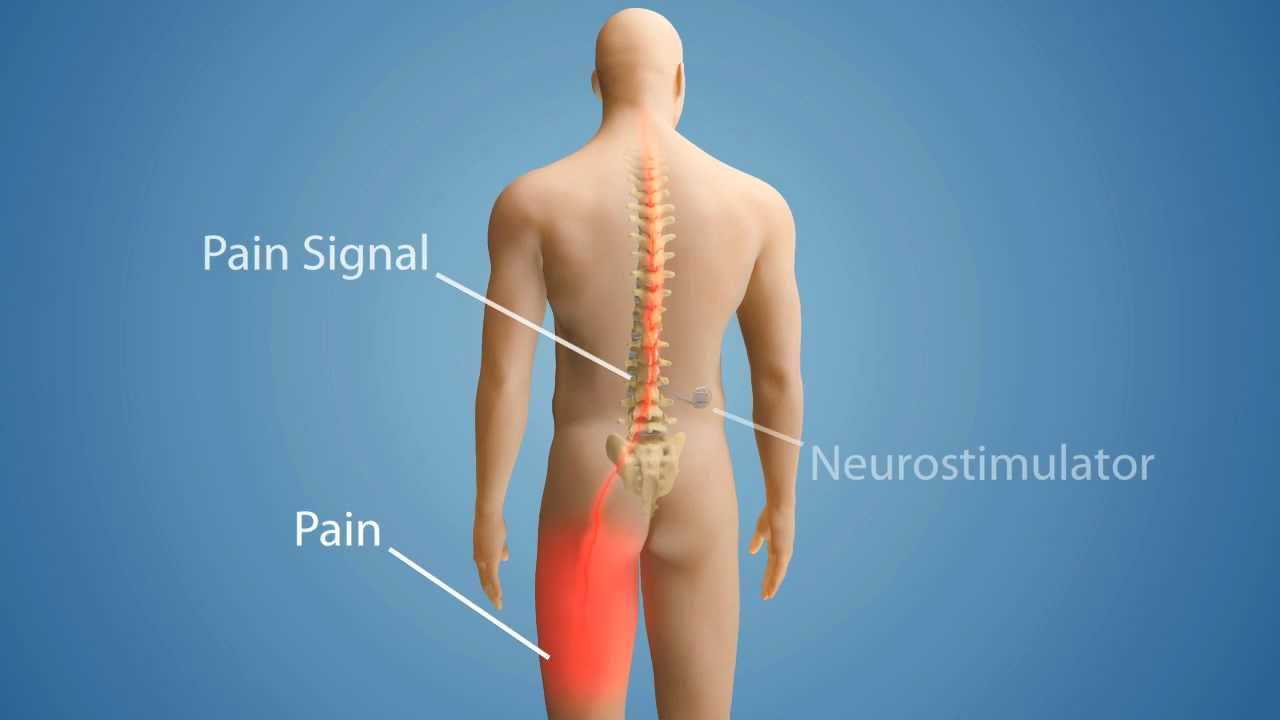
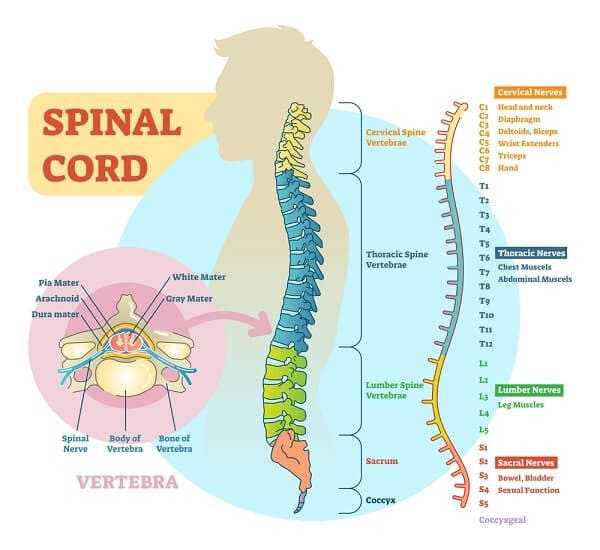
Spinal cord stimulation (SCS) devices produce electrical signals that can help control chronic pain, including low back pain. The stimulating electrodes are implanted in the epidural space as the appropriate spinal level, with an electrical pulse generator placed in the lower abdomen of gluteal area, and conducting wires connected to the generator and the remote control for the generator.
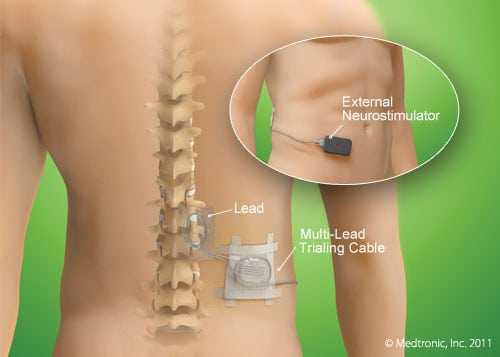
Positioning a Spinal Cord Stimulator
A five to seven day trial is typical for SCS in order to see if the device helps to relieve pan significantly. If so, the electrodes are permanently attached to the ligaments supporting the spine and the pulse generator is positioned and connected with supporting wires. Many patients are surprised at how SCS devices are positioned as the active site of pain is often much higher than they think. For example, those with sciatic nerve pain, which is experienced at L5/S1 usually requires an SCS to be fitted at T10.
When SCS is Used
Spinal cord stimulation devices are typically used for patients who have intractable neuropathic pain due to failed back surgery syndrome, complex regional pain syndrome and/or pain related to ischemia.