Stabilization Back Surgery in the Cervical Spine

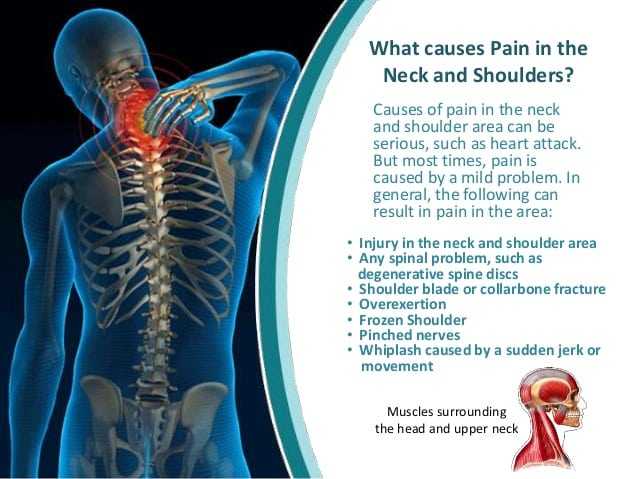
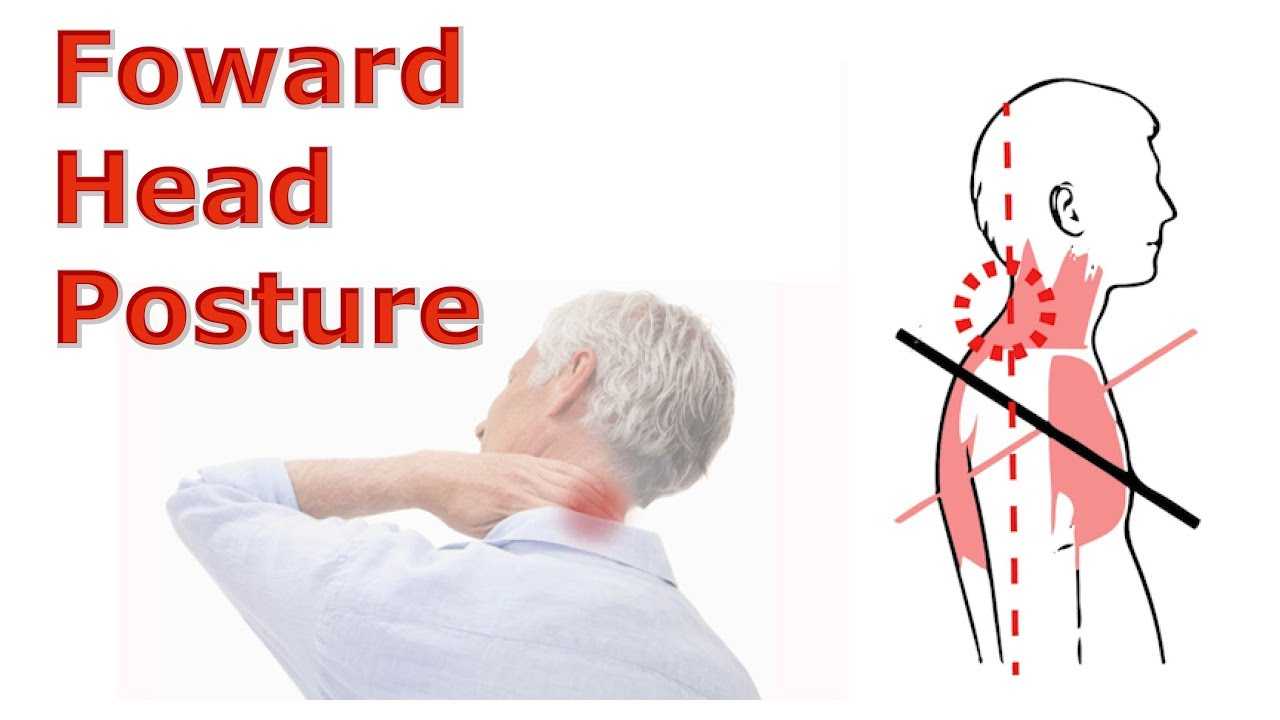
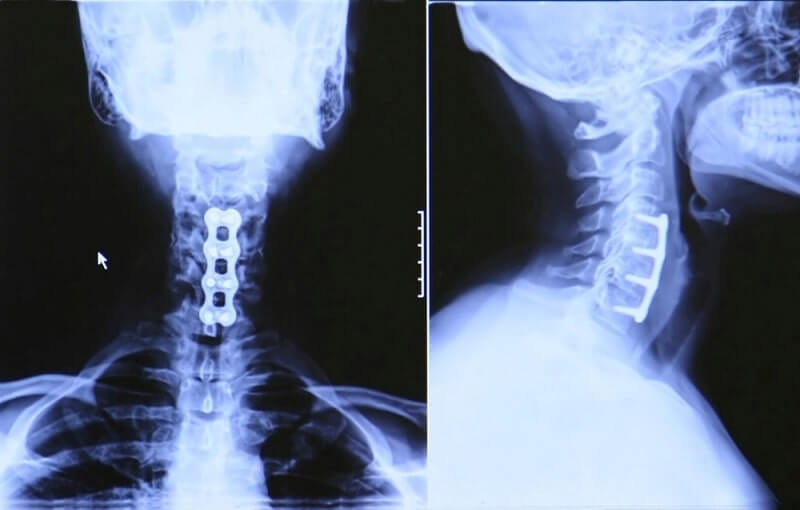
Some spinal surgeries on the neck involve stabilization alone as acute trauma, or spinal abnormality may be at risk of causing nerve compression due to improper spinal alignment. Realignment and stabilization in themselves may help decompress the spinal nerves and cord, such as in neck surgery for rheumatoid arthritis where the vertebrae may be fused in the upper neck to correct basilar invagination or atlantoaxial instability. Cervical facet joint disease (osteoarthritis) may also require spinal fusion after the diseased facet joint is removed to decompress the spinal nerves and cord. Although the facet joints themselves do not contain free nerve endings, they are innervated by mechanoreceptors, of which there are more in the cervical spine compared to the lumbar spine. This can mean that neck pain is considered more likely due to facet joint disease in the neck rather than the lower back. Many people with whiplash have evidence of cervical facet joint disease and suffer chronic neck pain because of this.
Laminotomy, Laminectomy, and Foraminotomy
If spinal nerve compression and spinal cord compression are present at the back of the spine then a surgeon will likely use a technique such as a laminotomy, laminectomy, or laminoplasty to decompress the cervical spine. The first two of the three procedures involve the excision of a portion of the backbone (lamina) in order to create space at the back of the spine into which the cord and nerves can relax. A laminectomy is more extensive and may require spinal fusion in order to maintain the stability of the neck after a large portion of the lamina is removed. A laminotomy may be combined with a foraminotomy in order to remove osteophytes or disc material impinging on the spinal nerves as they exit the spinal column. In a laminoplasty the surgeon cuts one side of the lamina and folds it back to create a hinged effect. Metal instrumentation is used to hold the ‘door’ in place and give the whole spine more space in which to decompress. This procedure can be advantageous in providing a good degree of decompression without actually removing any structural material and compromising the cervical spine’s stability.
Percutaneous Radiofrequency Neurotomy
Percutaneous radiofrequency neurotomy is another procedure that patients may choose to address the neck pain associated with whiplash and other neck trauma. This procedure denervates the facet joint through coagulation of the medial branch of the dorsal ramus. However, the nerve is not destroyed because the medial branch cell bodies remain intact in the dorsal root ganglion. The procedure does prevent the pain signals transmitting along the nerve to the dorsal root ganglion until the nerve grows back within 6-9 months (in most cases). At this point the neurotomy can be repeated as it is an effective method of pain relief in most (c70%) sufferers of whiplash-induced cervical facet joint disease. Multiple procedures can provide effective treatment for many years without the need for other, more invasive, surgery.
Minimally Invasive Cervical Spinal Surgery
Minimally invasive back surgery on the cervical spine is also an option for many patients and can provide a lower degree of risk for complications such as blood loss, bruising, trauma, and thrombophlebitis. It is usual for patients undergoing surgery on the neck to have the procedure performed whilst under a general anaesthetic in order to reduce the risk of them moving around during surgery in such a delicate area. Patients may have their head held still in a clamp during the procedure, which can cause trauma to the facial nerves or irritation to the skin. The recovery from a minimally invasive procedure is usually much shorter and, as muscles and ligaments usually do not require severing in these procedures, the risks of instability following such surgery are often reduced in comparison to traditional open procedures.