Additional Help for Persistent Symptoms

Even when you are receiving the best possible Parkinson’s disease treatment from your health care team, you may have persistent symptoms that interfere with your ability to function on a day-to-day basis. But there are solutions worth considering that can help minimize—or even eliminate—some of the more common persistent health challenges.
DYSKINESIA
One of the most bothersome symptoms for Parkinson’s patients is dyskinesia, the term used to describe irregular writhing, dancelike movements. If fast, these movements are called chorea; if slower, are called athetosis; and if very slowed, with posturing of a limb, neck, or trunk, are called dystonia.
Dyskinesia is not actually a symptom of Parkinson’s disease. Rather, it is a side effect from long-term use of car-bidopa/levodopa and can sometimes result from use of the dopamine agonist drugs. One recent study reported that a review of the medical literature over the past thirty-four years found that one-third of Parkinsons patients developed dyskinesia four to six years after starting carbidopa/levodopa therapy, and almost 90 percent developed dyskinesia after nine or more years.
Treatment of dyskinesia typically involves adjustment of the medications used to treat Parkinson’s disease. In cases where dyskinesia is severe and medication adjustments have failed to work, surgical treatment with either pallidotomy or deep brain stimulation can be very beneficial, by reducing the amount of dyskinesia up to 90 percent.
Treatment approaches to lessen dyskinesia include the following:
• Lower the dose of carbidopa/levodopa.
• Add a dopamine agonist to carbidopa/levodopa.
• Change from carbidopa/levodopa CR/ER form to the immediate-release form. • Add Symmetrel (amantadine).
• Lower the dose of carbidopa/levodopa and add a COMT inhibitor.
• Consider surgery (DBS or pallidotomy).
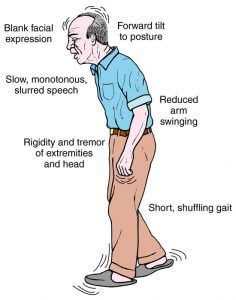
SPEAKING AND SWALLOWING PROBLEMS
The majority of people with Parkinson’s disease have some form of speech problems, even with drug treatment. Some of the more common challenges include
• A reduction in the vocal volume;
• A voice that fades out as you keep talking;
• Monotonous pitch that lacks expressiveness or changes in tone;
• Hoarse or breathy speaking voice;
• Poor articulation, with slurring;
• Rapid speaking, running together words without stopping; and
• Hesitation when beginning to speak or starting sentences.

The key with speaking problems is to work on them as soon as they appear. If you work with a conventional speech therapist or pathologist as soon as speech difficulties appear, you can learn exercises to deal with these various concerns, and help minimize further worsening of speech problems. But once speech problems are substantial, therapy can only help to some extent. Speech therapists may also focus on exercises for breathing, and tongue, lip, and jaw exercises. These can all help with loudness of the voice and also help correct some respiratory problems.
Collagen injections are another option when there is vocal cord weakness contributing to speech problems. Collagen is a particular type of protein that is found underneath the skin. For this treatment, collagen is harvested either from cows or from the patient. Once an allergy test shows that there is no allergy to collagen, the fifteen-minute procedure can be provided. Treatment involves application of a spray anesthetic to throat and nostril. A thin, flexible tube is inserted into the nose and down the throat, allowing for a view of the vocal cords. A syringe containing the collagen is inserted through the side of the neck, and the collagen is injected into the vocal cords.
Collagen injections work by increasing the size of the vocal cords, so that the vocal cords that have been slowed by the Parkinson’s become fatter and closer together, which makes them more effective at generating sound.
Vocal cord implants are another option, when someone has lost their voice due to weakened vocal cords. The FDA-approved implants add volume to a weakened vocal cord by pushing it to the center of the voice box, where it can more effectively produce sound. The half-hour procedure, which is done with local anesthesia, involves the doctor testing particular devices in the vocal cord area, via a small opening made through the thyroid cartilage. The patient tests out his or her voice with each testing device, until the voice is identified by the patient as normal, and then the tester is removed and a same-size implant is inserted.
Some patients opt to use computer communication boards or a handheld microphone to amplify their voice rather than consider a surgical procedure that is not fully guaranteed to work.
Some patients with more advanced Parkinson’s disease can have difficulties with swallowing, evidenced by coughing, gagging, or choking on food. Speech therapists trained in swallowing disorders can help evaluate the situation and recommend solutions and techniques to help minimize the problem. Patients with persistent problems may also benefit from a swallow study and examination by a speech therapist and possibly a referral to a gastroenterologist, who may be able to evaluate and recommend additional treatments. Very rarely, people who have severe swallowing problems and recurrent secondary aspiration pneumonia or malnourishment may need to consider placement of a feeding tube (PEG tube) directly into the stomach. This is more commonly needed in progressive supranuclear palsy (PSP), one of the Parkinson-Plus syndromes.
FREEZE ATTACKS
Freezing, a temporary inability to move, occurs in an estimated 30 percent of Parkinson’s patients, usually later in the course of the condition. Its more common in those patients whose Parkinsons started out with problems related to walking and balance. The times when freezing is most likely to occur include
• When getting up from a chair or bed and starting to walk;
• When approaching a doorway or walking through a doorway;
• When going into a tight space or elevator;
• When going up and down steps or over curbs; and
• When turning.
The key to dealing with a freeze attack is to break the freeze, particularly before you might lose your balance and risk a fall. Some people find that what helps them is developing their own set of prompts or triggers for walking. Some tricks can be used to help break a freeze:
• Imagine a line (i.e., a line of tape or a painted finish line) on the floor, then try to step over it.
• Hum or imagine a marching tune or count rhythmically to yourself.
• Aim for tiles or marks on the floor.
• Place dark-colored adhesive tape on the floor to make lines to step over.
• Step over your partners foot.
• Rock from side to side to get started.
One technique that helps some people is to create visual markers in frequently traveled paths in the home. For example, marking frequently traveled routes such as from the living room to the kitchen, or from the bedroom to the bathroom, creates visual cues and markers that can help with freezing or hesitation.
If someone is there, have him or her put a foot in front of you so that you can step over it, or have them tap you on the shoulder, or ask them to give you a hand to help. For freeze attacks, canes can also be fitted with a “step-over,” which is a plastic attachment that extends out from the bottom of the cane and can serve as a visual cue, or with a drop-down lever that drops on the foot and may release a freeze.
One device that patients have found helpful with freezing is a special cane that is equipped with a laser pointer. In one research study, patients with Parkinson’s were tested, and told to point the laser in the direction they wanted to move, and then to focus on stepping on the beam. Most of the subjects showed significant improvements in mobility. Other studies have found that frequent use of a laser pointer may make the benefits less effective over time.
Adjusting medicines may help in some patients, to ensure proper dosage and proper timing of dosage to maximize “on”-time and minimize “off-times.
Some Parkinson’s disease patients have found that trained companion dogs can help with walking and, in particular, freezing. With freezing, patients can’t continue or initiate movement without some sort of physical cue. Companion dogs can be trained to actually provide this triggering cue, by tapping on a patient’s foot with their paws. Dogs can also help open doors, retrieve lost objects, and help with balance, and help patients get back up after a fall. Working with a well-trained dog can reduce falls from 75 to 80 percent, according to research reported on in the National Parkinson Foundation’s Parkinson Report.
While some Parkinson’s patients are encouraged to get walkers, new research presented to the American Neurological Association in late 2001 found that walking aids such as walkers do not solve the problem of freezing. In research, Dr. Christopher Goetz of Rush Presbyterian-St. Luke’s Medical Center in Chicago had nineteen Parkinson’s patients follow an obstacle course. Dr. Goetz found that both standard and wheeled walkers slowed down the patients, and those patients using the walkers also had more freezing.
PREVENTING FALLS
Falls typically occur when Parkinson’s disease symptoms affect balance. When balance becomes unsteady, the ability to react is delayed, and stiffness and rigidity set in, reaction time can be affected, and falls can result. The most vulnerable times for falls include :
• When getting up from a chair;
• When sitting down in a chair;
• With the first step when starting to walk;
• When turning while walking; and
• When stepping on or off a curb or stair.
Walkers, particularly rolling walkers that have wheels, can be a help to some patients. However, some patients have a more difficult time with wheeled walkers, as they can go too fast and contribute to falling. If that occurs, removing the wheels and placing tennis balls on the ends of the four pegs will allow the person to slowly push the walker on a hard floor or firm carpet. In addition, some of the new large wheeled walkers have hand brakes and a seat so that the person can sit and rest when needed.
Canes, both standard and quad (with four legs that can stand on their own), can be a help to some people with walking. The benefit to a quad cane is that it’s always standing ready at chairside or bedside and is more stable.
High-heeled shoes can be a problem. Some practitioners believe the ideal shoe is a hightop sneaker, which provides better balance and ankle support. Also, if you tend to shuffle, you might want to switch to leather-soled shoes. They can be less sticky and are less likely to cause you to stumble than rubber soles.
Physical therapy from a therapist who specializes in balance can help improve posture and teach a Parkinson’s patient to use arms for balance and to take bigger steps—all techniques that can reduce the risk of falling.
Exercise—in particular, treadmill walking—can help strengthen legs, reduce stiffness, and help with general mobility. T’ai chi and yoga exercises that focus on centering one’s balance can be very helpful to improve balance and make body movements more efficient. All people with Parkinson’s disease should safety-proof their homes by removing throw rugs or any obstacles and installing grab bars and railings near the toilet, shower, bed, and stairs. Use of shower chairs and handheld detachable shower-heads may be a great benefit for those who have difficulty with balance. Also, simple changes in behavior, such as remembering to be seated when doing things like dressing, can prevent unnecessary falls.
SKIN CHANGES
Seborrheic dermatitis and dandruff, which are frequent side effects of Parkinson’s disease, can sometimes easily be treated by dandruff shampoos that contain salicylic acid and coal tars. Over-the-counter 1 percent hydrocortisone cream applied to the affected areas may greatly lessen flaking and itching of the scalp and forehead. Other prescription medicines such as ammonium lactate (Lac-Hydrin) may be helpful. If these therapies do not work, then consultation with a dermatologist should be sought.
HYPOTENSION, LIGHT-HEADEDNESS, AND FAINTING
A lowering of blood pressure upon standing can occur as a side effect from all of the medicines used to treat Parkinson’s disease, as well as from many blood pressure medicines, some antidepressants, and drugs used to treat bladder dysfunction. A review and adjustment of one’s medicines and evaluation by a cardiologist to rule out heart problems should be considered for recurrent fainting or near-fainting spells. Simple treatments to reduce light-headedness and near fainting include wearing support stockings, slowly rising from a lying or sitting position, placing blocks under the head of the bed, adding salt to one’s diet (if okayed by your doctor), and adding caffeinated beverages or over-the-counter tablets. Prescription drugs that can help treat fainting that results from lowering of blood pressure include fludrocortisone (Florinef), midodrine (Proama-tine), and indomethacin (Indocine).
EXCESSIVE SALIVA AND DROOLING (SIALORRHEA)
Excessive drooling may be reduced by taking carbidopa/ levodopa (Sinemet), dopamine agonists, and anticholinergic agents (Artane and Cogentin). In people who do not have a history or symptoms of heart disease, placing a few drops of atropine ophthalmic 1 percent solution on a spoon and then adding tap water and swishing and swallowing before bedtime may reduce nighttime and daytime drooling. In addition, injection of botulinum toxin into the salivary glands may be helpful in severe cases of sialorrhea.
CONSTIPATION
Constipation, which is defined as having fewer bowel movements than usual, with a long or hard passing of stools, is very common in Parkinsons disease. Anti-Parkinson drugs can cause constipation, so you should review your medicines with your physician. Remember that there is no “right” number of daily or weekly bowel movements. “Regularity” may mean bowel movements twice a day for some people or just twice a week for others. But if its determined that you are having constipation, there are a variety of things you can do to help deal with this situation.
• Drink enough water. You absolutely need to, at minimum, drink eight 8-ounce glassesof water-based, caffeine-free beverages. That could be water, caffeine-free herbal tea, or unsweetened seltzers.
• Increase the amount of fiber in your diet. Fiber is also beneficial in helping speed up the response to levodopa. You can add fiber by increasing your intake of fresh fruits and vegetables, either cooked or raw, as well as whole-grain cereals and breads. Dried fruit such as apricots, prunes, and figs are especially high in fiber.
• Avoid high-fat meats, dairy products, sugary desserts, and excess consumption of eggs or convenience foods, which can all contribute to constipation.
• Don’t misuse laxatives or enemas. You may think of them as treatments for constipation, but laxatives and enemas should be used only on the advice of your physician, as they can be habit forming. If you rely on laxatives or enemas for too long, you may lose further bowel function and come to require them for elimination.
• Don’t ignore the urge to have a bowel movement. While you may prefer to have your bowel movements at home, waiting can worsen chronic constipation.
• Be as active as possible. Physical activity helps contribute to normal bowel function, so get as much exercise or walking in as you possibly can.
• Consider adding bran to your diet. Unprocessed bran, also known as miller’s bran, can be added to baked goods, cereals, and fruit. If you add bran, introduce it slowly, as it can cause some bloating and gas while your digestive system adjusts.
• Another remedy is also absolutely worth mentioning here. A basic and classic Ayurvedic herbal remedy known as triphala has been found to help digestion and constipation problems. Various triphala preparations are available at many natural health and vitamin stores, but a particularly reliable brand is Planetary Formulas Triphala.
If all of the above remedies have failed to regulate your bowel movements, you might try over-the-counter bulk agents like psyllium (Metamucil), methylcellulose (Citrucel), or docusate (Colace). These may need to be taken at twice the recommended dose in persons with Parkinson’s disease in order to be effective. If this fails, then a prescription medication such as Lactulose or Miralax may be very effective in relieving constipation.
INCONTINENCE
Incontinence refers to either the inability to hold urine or feces until you reach a toilet, or leakage due to stress or overflow.
If you are experiencing incontinence, you may try to hide the problem from friends, family, and even your doctor. But there are many options to treat and control, even cure the situation, so you need to speak up and bring this to the attention of your physician. This discussion and medical assessment by your doctor should be your first step. The doctor may refer you to a urologist, a doctor who specializes in diseases of the urinary tract, or to a gynecologist, a specialist in the female reproductive system.
There are some things that can be done to help treat incontinence:
• Behavioral techniques such as exercises for pelvic muscles, biofeedback, and training the bladder to control urination can help you wait until you can reach a toilet.
• Some medicines can be prescribed that treat incontinence, including oxybutinin (Ditropan), tolterodine tartrate (De-trol), and prazosin (Hytrin).
• Sometimes surgery can improve or cure incontinence if it is caused by a structural problem such as an abnormally positioned bladder or a prostate enlargement.
• Another option for serious and persistent bladder problems is what’s known as a bladder pacemaker. This device is surgically implanted under the skin, in the lower-abdomen area. A wire containing electrodes is inserted at the base of the spine, near the nerves that regulate bladder function. The pacemaker sends painless electrical signals to the bladder to contract or relax as urine is stored or eliminated. In clinical trials, the pacemaker reduced leakage in 74 percent of patients within six months, and almost 50 percent of patients had no accidents or leakage at all.
When incontinence cannot be cured, there are some techniques to help manage the situation. For example, special absorbent pads can be used. Also, absorbent and even disposable underclothing, no more bulky than regular underwear, can be worn under your clothing. Also, in some cases, a flexible tube, known as an indwelling catheter, may be a solution. The catheter is inserted into the urethra, and urine is collected in a container. Men also can use an external collecting device that is fitted over the penis and is connected to a drainage bag, called a condom catheter. This can be very helpful for men who need to urinate frequently at night.
Although Parkinsons disease and its effect on the autonomic nervous system can cause incontinence, this problem can also occur as a side effect of some medicines or as a symptom of a bladder or urinary tract infection. (A sign of infection would be burning pain upon urination and possibly an unpleasant odor to the urine.) If you have difficulty with your bladder function, review all of your medications to be sure they are not the cause or contributing to your symptoms. Your physician can easily rule out an infection by checking a culture with a clean urine sample, and a urologist can perform an exam and tests to check for enlarged prostate or bladder prolapse, which can sometimes be the cause of these symptoms.
SEXUAL DIFFICULTIES
Problems with sexual function may also occur as part of Parkinson’s disease, resulting from the disruption of normal function of the autonomic nerves that regulate sexual function of the body. This is very common and probably vastly under-reported, due to the sensitive nature of the subject. Sexuality is a vital part of everyone’s life and should be addressed and taken seriously, like all symptoms. If you are having a decrease in your sex drive or have the desire but cannot fully achieve and maintain an erection or reach orgasm, discuss your concerns with your physician. Your physician can evaluate you further to rule out other illnesses and conditions that can cause sexual problems, such as diabetes, hypothyroidism, poor blood circulation, hormonal imbalances, and depression. Your family doctor can perform simple blood tests to check for some of these and might refer you to a urologist or gynecologist for further evaluation. A long list of medicines can cause impotence, including some blood pressure medicines, especially beta-blockers, anticholinergics (Artane, Cogentin), sedatives, antianxiety and antidepressant agents, and antihistamines, among many others. Your physician can evaluate your medicines to determine if any of them may be contributing to sexual problems. It’s also important to note that alcohol in excessive amounts can cause impotence.
Impotence may be effectively treated with a variety of medicines such as sildenafil (Viagra), which is very effective for men with Parkinson’s disease, and possibly for women as well. One note of caution: Viagra should not be used in men or women who have serious active heart disease or who are taking nitrates. Other oral medications that can reduce impotence include yohimbine (Yocon) and bromocriptine (Parlodel), if prolactin levels are elevated. Injections directly into the penis with papaverine HCL (Papaverine), phentolamine (Regitine), or al-prostadil (Caverject) may improve erections in 65 percent of all men regardless of the cause of impotence.
FATIGUE AND SLEEP PROBLEMS
Fatigue is a common problem with Parkinson’s patients. In some cases, the fatigue is actually from medications being taken. One study, conducted by Dr. Mahyar Etminan from the University of Toronto, found that patients who take ropinirole (Requip) and pramipexole (Mirapex) have a five times greater risk of sleepiness, compared with those taking placebo drugs. Patients are also more at risk of sudden “sleep attacks,” in which extreme sleepiness comes on rapidly. The sleepiness that came from these drugs also put some patients more at risk of automobile accidents. The researchers said that physicians should make their patients aware of this side effect and advise patients who feel drowsy while taking ropinirole or pramipexole not to drive.
Frequently, however, the fatigue is either just a side effect of the condition overall, or the result of aging-related disturbances that are exacerbated by the Parkinson’s disease. Insomnia is one of the most common complaints about sleep. Insomnia can refer to taking too long a time to fall asleep— i.e., more than thirty to forty-five minutes—or waking up many times each night. Insomnia can also include waking up early and being unable to get back to sleep, and waking up feeling tired.
If you are having insomnia, one of the first things you need to have evaluated is whether you may have sleep apnea. Apnea is a common problem that causes your breathing to stop for periods of up to two minutes, often many times each night. Apnea can be due to some sort of obstruction—air can’t flow in or out of the nose or mouth—which is called obstructive apnea. Or, it can be central apnea, which is less common, and takes place when the brain doesn’t send proper signals to start the breathing muscles. The combination of daytime sleepiness and loud snoring at night is a sign that you might have sleep apnea and should see a physician specializing in sleep disorders. Treatments for apnea include a change in sleeping position, devices to keep the airways open with supplemental oxygen at night, medication, and surgery.
When insomnia is not due to apnea, it can be helped by a variety of approaches.
• First, try to follow a regular sleeping schedule, going to sleep and getting up at the same time.
• Keep daytime naps to a minimum.
• Get regular exercise daily.
• Expose yourself to natural afternoon sunlight every day.
• Don’t drink caffeinated beverages late in the day or evening.
• Avoid drinking alcohol late in the day or evening.
• Create a safe and comfortable place to sleep. The room should be dark, well-ventilated, and quiet.
• Develop a bedtime routine, which could include reading, a bath, or other relaxing activity.
• Use your bedroom only for sleeping.
If these techniques don’t work, and you suffer insomnia for more than several weeks, it’s time to discuss options with your practitioner. Natural or holistic practitioners may advise the use of melatonin or the herb kava kava as a sleep aid. Conventional practitioners have a variety of sleep-inducing drugs that may be of help to Parkinson’s patients.
Older Parkinson’s patients should be particularly careful about over-the-counter sleep aids that contain the drug diphenhydramine as an active ingredient, however. Products such as Sominex and Benadryl contain diphenhydramine, and researchers have found that the ingredient dramatically increases the risk of symptoms of delirium and dementia in patients age 70 or older. These may be very effective in younger persons, however. Tylenol PM is a fairly safe drug and may help one to sleep better. Sometimes it is necessary to add a short-acting sedative prescription medication (i.e., Ambien, Ativan). Another common cause of sleep disturbance in Parkinson’s patients is “restless legs syndrome” (RLS). This syndrome can cause crawly, prickly sensations, primarily in the legs, but sometimes affecting the arms and trunk. These sensations are more common and severe at night, are usually relieved by moving the legs, and can cause legs to jerk involuntarily during sleep—and sometimes even when awake. RLS may make it hard to fall asleep or may wake you up frequently. Besides the recommendations for better sleep offered earlier in this section, the main drug treatments offered for restless legs syndrome are the dopamine-receptor agonist drugs, such as pramipexole (Mirapex), pergolide (Permax), and ropinirole (Requip), but also carbidopa/levodopa. Sedatives, such as the mild tranquilizer clonazepam (Klonopin), can be effective as nighttime treatments in some people. In people who have ongoing RLS, some doctors recommend pain relievers, such as propoxyphene (Darvon), oxycodone (Percocet), or hydrocodone (Vicodin). Anticonvulsants, in particular neu-rontin (Gabapentin), are also used in some patients who have extensive daytime symptoms and pain associated with their RLS.
DEPRESSION
Everyone feels a bit down here and there, but when having a case of the blues persists, and interferes with your ability to function, then it’s time to take a look at whether or not you might have clinical depression.

Symptoms of depression include the following:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness, pessimism
- Feelings of guilt, worthlessness, helplessness
- Loss of interest or pleasure in hobbies and activities that were once enjoyed, including sex
- Decreased energy, fatigue, being “slowed down”
- Difficulty concentrating, remembering, making decisions
- Insomnia, early-morning awakening, or oversleeping
- Appetite and/or weight loss or overeating and weight gain
- Thoughts of death or suicide; suicide attempts Restlessness, irritability
- Persistent physical symptoms that do not respond to treatment, such as headaches, digestive disorders, and chronic pain
Unfortunately, many of these symptoms may be dismissed— even by you, your doctor, family members, or a caretaker—as symptoms of “old age” or may be assumed to go along with the Parkinson’s disease. But clinical depression can occur at any age and can exist alongside but separate from Parkinson’s disease, so if you have these symptoms, you should talk to your doctor about being evaluated for depression.
Long-term, clinical depression may require antidepressant therapy (i.e., nortriptyline [Pamelor], sertraline [Zoloft], paroxetine [Paxil], citralopram [Celexa], venlafaxine [Effexor], mirtazapine [Remeron], or bupropion [Welbutrin]) in combination with talk therapy or psychotherapy. In cases of severe, catatonic depression, admission to the hospital and possible treatment with electroconvulsive therapy in addition to antidepressant medicine may be necessary. Milder depression can frequently respond to therapy, aerobic exercise, support groups, and herbal supplements, such as St. John’s wort.
But the critical first step is to admit that help is needed. Mental illness is an uncomfortable topic for some people, and some people mistakenly believe that it is a sign of weakness to ask for mental health help and that one should be able to just “snap out of it” when depressed. But depression is a physical problem and deserves medical attention, not embarrassment. The first step in dealing with depression is a discussion with your general-practice or primary care doctor—which may be your neurologist—for an assessment. The doctor will evaluate for any other medical or drug-related causes for depression and should conduct a complete review of the medicines you are taking, along with blood tests for thyroid function (thyroid panel), a complete blood count (CBC), and a check of your vitamin B12 level. The doctor can then make a referral to a mental health specialist—i.e., a therapist, counselor, psychologist, or even one of a new type of specialist, a geriatric psychiatrist—for further assessment and treatment.
WRITING PROBLEMS
The medicines used to treat Parkinson’s disease usually help to improve micrographia (small and/or illegible handwriting). In addition to medication, there are various approaches you can take to help with this problem.
First, some people find that specialized occupational therapy geared toward writing and manipulating objects by hand can be of help.
Specialty stores and online outlets also sell a variety of writing aids, including special extra-wide “fat” pens and pens with special grips that make them easier to hold and write with.
Some people can obtain similar results by putting rubber bands on pens to make them fatter and easier to grip. If you have difficulty signing your name, you can ask your local bank to make a signature stamp for you that you can legally use for signing your checks.
Finally, some people have found that a computer, typewriter, or handheld pointer-input device—such as a Palm Pilot handheld computer—may be easier than handwriting for some tasks.
Inexpensive and effective voice-activation software can even make “typing” easier for those with limited dexterity or typing skills.
DEMENTIA, MEMORY, AND COGNITION
Memory loss is a problem for some Parkinson’s patients. In the past, this was written off as a sign of aging, but it’s now known that severe memory loss and confusion are not a normal part of aging. While some memory lapses or slowness in remembering certain details can be fairly benign and is somewhat common in Parkinson’s disease, some patients will have more significant changes in memory, personality, and behavior that are characterized as dementia. The term dementia describes various symptoms that include repeating the same questions, becoming lost in familiar places, inability to follow directions, being disoriented, and neglecting safety, hygiene, and nutrition.
If you are concerned about memory and cognitive problems, your first step is to visit your primary care doctor or neurologist, for a complete medical examination to assess any identifiable causes. Be sure to review all of the medicine you are taking, because many medicines, including the ones for Parkinson’s, can cause mental slowing and confusion. Virtually all of the medicines that are used to treat Parkinson’s disease can cause side effects of mental dulling, confusion, and even hallucinations. Although carbidopa/levodopa (Sinemet) and the dopamine agonists can do this, the more notorious medicines that should be tapered off and stopped in cases of dementia with Parkinson’s disease are the anticholinergics (trihexyphenidyl [Artane], benztropine mesylate [Cogentin], amantadine [Symmetrel], and selegiline [Eldepryl]). Other medicines that may also contribute to impaired thinking include those that treat bladder problems, high blood pressure, depression, anxiety, or insomnia.
In addition, standard tests may be done to evaluate memory problems, including a brain scan (CAT scan or MRI) and an EEG (electroencephalogram) or brain wave test. Common blood tests are also done, including thyroid studies, vitamin B 12 levels, a screen for syphilis called an RPR or VDRL, as well as a routine blood count called a CBC and a chemistry panel to check for proper liver and kidney function. These tests are used to rule out other possible causes of dementia such as low thyroid levels, small strokes, and B 12 deficiency. If a sudden change in behavior or thinking occurs, in addition to reviewing the medications, a physical exam and a screen for infection (of the urine or lungs) should be performed. You may also be referred to a psychologist for cognitive testing that involves several hours of pencil-and-paper questions to check your memory, verbal, and problemsolving skills.
If no specific cause is found for memory problems, some experts suggest incorporating daily activities to keep the mind and memory sharp. These activities can include hobbies or projects, crossword puzzles, exercise, and other interests.
When memory becomes less reliable, it becomes more important to make to-do lists and to keep a calendar and notepad with you at all times in order to jot down schedules, events, and things to remember. Some people prefer small electronic organizers or handheld computers.
Medications that have been proven to help in the dementia of Alzheimer’s disease may also be very helpful in treating dementia found in persons with Parkinson’s disease. These medicines—donepezil HCL (Aricept), rivastigmine tartrate (Excelon), and galantamine (Reminyl)—act by increasing the chemical acetylcholine in the brain and may improve memory and concentration.
If a person is having frequent hallucinations, and a complete physical examination and review and adjustment of medications fails to find a cause or relieve their presence, then treatment with atypical antipsychotic medicines such as queti-apine (Seroquel) or clozapine (Clozaril) should be considered.