Understanding Sjogren’s Syndrome
Sjogren’s is a multisystem disease. However, it is not the most far-reaching disease of all the autoimmune conditions. The winner of that dubious distinction, as we have seen, is lupus. (In this case, Sjogren’s will have to settle for the silver medal.) Sjogren’s can be both primary and secondary diseases. It can appear, for example, along with and secondary to rheumatoid arthritis, polymyositis, and scleroderma in addition to lupus, as mentioned earlier.
One of the most bizarre and I think one of the most important aspects of this illness in terms of research is the greatly increased risk that Sjogren’s patients have of developing lymphoma—that is, cancer of the lymph system. The lymph system—that complex of liquids and cells that are an integral part of the immune system—is the highway of immune function. We know for sure that the lifetime risk of developing lymphoma goes up about forty times upon a diagnosis of Sjogren’s. For this reason, if no other, I advise all my patients with this disease to get frequent medical checkups (at least yearly) and to report any new and more unusual symptoms, particularly swollen glands. The most common place for lymphoma to develop in people with Sjogren’s is in the salivary gland. Other lymphoma-induced symptoms may include fever and tiredness, itchy skin, and unexplained weight loss.
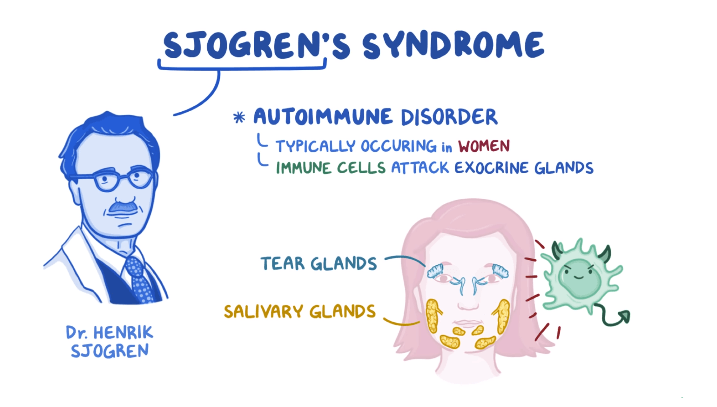
Sjogren’s syndrome was first mentioned, although not by that name, in 1888. A Polish surgeon, Dr. Johannes Freiherr von Mikulicz-Radecki, found cells of the lymphocyte type had filtered into the parotids (saliva-producing glands that are found in the cheeks) and lachrymal (tear-producing) glands of a farmer. Then, in 1933, a Swedish eye doctor, Henrik Sjogren, described the initial disease triad of parotid enlargement, lack of saliva, and dry eyes, and the disease was given his name. Now, more than eighty six years later, we have learned much, though hardly enough, about the disease and its etiology.
Causes of Sjogren’s Syndrome
Those who study this disease believe it is probably caused by a combination of factors, including genetics, infection, and the environment. I use the word “believe” because no one yet has been able to link a specific gene to the Sjogren’s. Current research shows that several different genes appear to be involved and can predispose different people to the disease, but none of them alone, as far as we know, causes Sjogren’s. Some sort of trigger must activate the immune system first. I believe these triggers most likely are either bacterial or viral in nature.
One prime candidate is the Epstein-Barr virus (EBV). EBV is known to stimulate the production of the rheumatoid factor, which is associated with Sjogren’s syndrome and lupus, as well as with rheumatoid arthritis. It may be that that particular virus stimulates the immune system and then the gene alters the way the immune system responds. In other words, in the process of attacking the virus, the misguided lymphocytes also go to the moisture glands and there attack the healthy cells, provoking inflammation and ultimately damaging the glands.
There is another association that bears mention and leads me to believe that this disease is caused by a virus. Fairly recently, a new condition was described in people infected with the HIV virus that was originally thought to be Sjogren’s syndrome. This condition is called diffuse infiltrative lymphocytosis syndrome (DILS). DILS symptoms look exactly like those related to Sjogren’s syndrome; the enlarged parotid glands and dry eyes, mouth, and mucous membranes are all a part of this condition. The difference is in the physiology of the disease. In DILS, it is the suppressor T cells that operate, instead of the helper T cells that work in regular Sjogren’s syndrome. While Sjogren’s is only assumed to be connected to a virus, albeit one that we cannot yet identify, the HIV-infected patient is known to have a true virus as the cause of the disease. The fact that DILS is unrelated to Sjogren’s syndrome but has identical characteristics may be Mother Nature’s way of telling us that Sjogren’s is really caused by a virus. It is only a theory, but I believe it’s a valid one.
Living with Sjogren’s
Living with Sjogren’s can be challenging. If the dry eyes persist despite medication, the drainage end of the tear ducts may have to be plugged surgically to keep the eyes moist. Creams and lubricants in the vagina and artificial saliva provide moisture, as mentioned above, and this seems to be sufficient for many. Patients who are very severely affected have great difficulty, however. Their eyes are chronically bloodshot and they have to wear goggles for protection. When surgery or artificial tears and saliva do not work, some patients take drugs, such as the pilocarpine preparation mentioned above, that induce as much moisture as possible, but often their mouths still are parched at times.

Sjogren’s patients generally require additional drugs, such as prednisone, to keep their immune systems in check and at least allow a modicum of tears and saliva. This treatment may be necessary for a lifetime. Almost all of the patients with Sjogren’s are seeing psychiatrists or psychologists, not necessarily because of depression, but rather because the antibody has an effect on how their minds work. It is not an easy thing to live with this disease, but I have many people who, despite the difficulties, continue to lead productive and enjoyable lives.