Vaginal Pain

THE FOLLOWING ARTICLE CONTAINS ANATOMICAL IMAGES THAT ARE FOR ADULT AUDIENCES ONLY.
A discussion of this type is very daunting to me. After practicing Internal Medicine for over 26 years (the later years of my career exclusively in the treatment of chronic pain), I can think of few disorders that challenged me at so many different levels and in so many ways.
I feel inadequate to expound on this topic. Nevertheless, this article will be my approach to the woman with vaginal pain. I will endeavor to explain this mysterious topic. My approach will be like that of a medical detective…methodical and detailed.
This article will not be an exhaustive evaluation of the causes of pain in the female pelvis (click here to see a previous post of mine on female pelvic pain). I will be restricting my discussion on the causes of pain of the vagina and associated structures. The medical term for this is vulvodynia.
Consider The Female Anatomy And Physiology
A discussion of this type should always begin with an understanding of the intricacies of female anatomy and physiology. The female pelvic anatomy is very complicated. After neuro-anatomy and facial anatomy, I believe it is the third most complicated anatomic-physiology of the human body.
The anatomy and physiology present a challenge for a number of reasons:
- The pelvic organs are very compact. There are many organs that lie very closely to each other in the female pelvis. Each has a unique blood, nervous, and lymphatic supply. Disruption of one organ system often effects its neighbor given the close proximity of things.
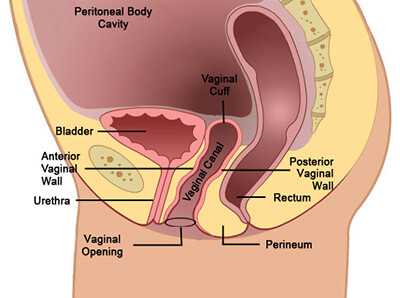
- It is difficult to design effective diagnostic tools for this region of a woman’s body. The boney pelvis “camouflages” the contained organs from our diagnostic studies. Furthermore, even with direct inspection, the “tightness” of the anatomy challenges all but the most meticulous surgeons. It is easy to “miss” an abnormality even on direct inspection surgically (such as with a laparoscope).
- This area often expands and contracts dramatically in the process called pregnancy. Though a “normal” process, the resultant disturbance to a woman’s anatomy can leave permanent injury with scarring.
- Even in a woman who has never been pregnant, the usual monthly menses is really a process of inflammation, hemorrhage, and healing. This means that the female reproductive system is in a “normal” state of cyclic injury and healing.
- The vagina is the only portal in the human body where a sterile space (the female peritoneal cavity) is in direct connection with the unsterile outside (the vaginal opening called the introitus). The access for infection from the vagina to the sterile interior of a woman’s abdomen is part of her normal anatomical arrangement.
- Sexual intercourse challenges the resilience of this system even further. The activity increases infectious “seeding” many fold over what her vaginal portal already threatens.
- The vagina provides a location for abnormalities to escape detection. Infections that are easily identified while on the male genitalia are often hidden deep within the recessed vagina.
And I could go on. Are you getting the idea of how challenging a woman’s anatomy and physiology is?
How To Diagnose The Cause Of Vaginal Pain
A reasonable first approach to the diagnosis of vaginal pain may be as follows:
If, after a meticulous work-up for the cause of vaginal pain, no obvious cause can be found then the “diagnosis” of VULVODYNIA is made. The exact cause of this malady is unknown. The symptoms may be itching, burning, throbbing, aching, or even a sense of fullness.
There may be pain that is constant or intermittent. The discomfort may be triggered or made worse with sexual intercourse (called dyspareunia). This syndrome may occur after a Hysterectomy (surgical removal of the uterus) or occur with sexual abuse.
The exact mechanism for vulvodynia remains elusive. There is some experimental evidence that it is a form of pelvic neuropathy. Other studies seem to implicate spasm of the muscles of the floor of the pelvis.
Besides sexual intercourse, bicycle riding and pregnancy may also worsen vulvodynia. Essentially anything that increases neural activity and blood flow to the vagina worsens pain. The following is a good approach to the diagnosis of vulvodynia:
How To Treat Vaginal Pain ?
Naturally, any identified cause for vaginal pain should be treated directly. Serious disorders should be ruled out as a first priority. The appropriate treatment will usually cause the vaginal pain to resolve.
In the cases where no real causative disorder can be found, or the appropriate treatment of an identified disorder does not relieve the vaginal pain, the following general treatments have been found to be helpful relieving vulvodynia:
- Rinsing the vulva (external female genitalia) with cool water after urination or sexual intercourse.
- Soaking in warm or cool Sitz baths (a small tub of water that inserts into the opening of a toilet seat and has a stream of water fed from a suspended bag).
- Ice packs wrapped in a towel applied to the genitalia.
- Using mild, unscented soaps and detergents.
- Using white, unscented toilet paper.
- Wearing white cotton underwear.
- Wearing loose fitting clothing.
- Avoiding the use of panty hose and tight fitting garments.
- Avoiding activities that worsen the pain (such as bicycle riding).
- Avoid pools and hot tubs with chlorinated water.
- Avoid foods that worsen the discomfort (such as berries or chocolate).
The following therapies have been shown to be helpful with reducing vulvodynia:
1) Topical Estrogen Creams
2) Topical Anesthetics
3) Anti-depressants (such as Elavil)
4) Anti-convulsants (such as Lyrica)
5) Biofeedback (click here to see my recent post on this subject)
6) Surgical treatment (if scar tissue is present in the vagina)
7) Complementary and Alternative Treatments (click here to see my post on this subject)
This is not an exhaustive listing of all therapies but does give you an idea how expansive the therapy for vulvodynia can be.
There Is Hope…
I have reviewed the causes for vaginal pain as well as the mysterious “vulvodynia.” The treatments are useful at reducing the symptoms even if not curative. Identifying an exact cause can be very challenging such that symptomatic treatment is often the most practical approach for the patient. I hope you have found this article helpful.
Remember…the beginning of the search for the cause of vaginal pain is an evaluation by a well-trained health care practitioner.
Don’t forget to send me comment and question. I would love to hear from you and will answer you back promptly.
Wishing you much joy and good health,