What can I do to avoid surgery for my herniated disc?

You have been told that you have a herniated disc on your MRI scan and that you need surgery, but you are getting around all right and you do not have severe pain, weakness, or loss of bowel and bladder function forcing you to have emergency surgery. What are your options? Most people with disc herniations fall into this category. They can get around, but that is about it. Something must be done so that they can sleep, go to work, and eventually get back to normal.
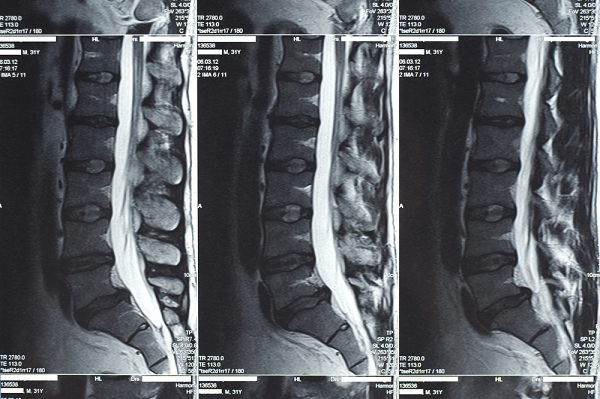
First of all, it has been proven that if you can live through the pain without surgery, you have better than an 80 percent chance of full recovery (no pain, full function, no nerve damage) within one year and 92 percent in 10 years. This is the same chance of recovery that you can expect with surgery! It seems obvious that waiting is safer than having surgery. But that is not necessarily true if you develop a complication from nonoperative treatment, such as becoming habituated to pain medications, developing a bleeding ulcer from anti-inflammatory medication, or developing an infection from an injection. So then what is the safest and most effective course of action: surgery or no surgery?

I advise my patients who have a painful disc herniation that they have three options. The first is to walk it off and be as active as you can be within the limits of the pain. I reassure them that there is a good chance the disc will shrink by itself, given enough time, and that the pain will go away within four months of onset. Our bodies have normal defense mechanisms that allow this to happen. If their pain is not interfering with their sleep and work, they usually take this option. After such discussions, many a patient has told me that understanding the problem was half the cure. Knowledge of the natural history of disc herniation gave them the reassurance they needed to discontinue medical care and walk it off!
If they require pain relief in order to sleep and function, I recommend a series of one to three epidural steroid injections (I will explain what epidurals are in a moment). Epidurals are very effective in relieving pain from a herniated disc. Pain relief allows you to walk off the symptoms and keeps you from taking narcotics and muscle relaxants (commonly prescribed pain relievers), which are habitforming, make you drowsy, and cause depression (more about chronic back pain). If the pain from a herniated disc is still significantly impairing their quality of life after three months of waiting for it to go away, then I recommend the third option, surgery. Here is a further explanation for the three options in treating a painful herniated disc: walk it off, epidural steroid injection, and surgery.
Related Article
Spinal Injections For Back Pain
What does it mean to “walk it off?”
We know from several classic studies that the natural history of symptoms from disc herniation is spontaneous resolution, if given enough time. As long as the disc has not caused progressive or severe nerve damage, it is better to try to walk the symptoms off. The secret is not to allow the pain to make you physically debilitated or mentally ill.
First you should consult a spinal specialist who is familiar with disc problems and who should determine that your symptoms are really the result of a herniated disc.
Second, you should do only what is necessary to obtain enough pain relief so that you can get a night’s sleep and get around enough to take care of yourself. This means taking as few narcotic painkillers and anti-inflammatory medications as possible. Try not to take any muscle relaxants at all, which cause too many side effects, such as drowsiness and depression. Avoid traction, hanging upside down, manipulation, and especially passive stretching of the painful extremity. Remember how I made an enemy of a colleague by performing a straight-leg-raising test? Very light massage, heat and/or ice packs — well padded so as not to burn your skin — are good for pain relief. Most of these touch measures, as well as acupuncture, will relieve pain as long as you are not taking narcotic pain medications. I will explain the reason for this in the chapter on chronic pain. Try to remain as active as possible within the limits of your pain and stamina. Walking, aquatic exercises, stationary bicycle, and treadmill aerobics all help to keep you from becoming deconditioned (out of shape). Do not take pain medication so that you can exercise. Remember that the pain is a warning that something is wrong, and it is a normal defense mechanism. If, because of the pain, you cannot remain active despite these measures, then you should consider the following options for your disc herniation.
What is an epidural, how does it work, and is it painful?
Epidural steroid injection (epidural) is a method of injecting a small amount of local anesthetic and steroid medication (the most powerful antiinflammatory drug available) directly into the area of your spine where the nerve is being irritated by the herniated disc. The object is to place the potent steroid where it will do the most good. The local anesthetic is added to the injection to give you immediate pain relief and to confirm that the injection is at the correct location. Herniated discs can be a triple whammy to the nerve because they not only compress and stretch the nerve, but they leak irritants to the nerve. Epidural steroid injections are meant to block the irritants and reduce the pain. I prescribe them so that patients can get enough pain relief to avoid taking narcotic painkillers and so that they can get a good night’s sleep. One of the benefits of epidural injections is that only small doses of steroids are required to be effective.
I am not an advocate of giving steroids by mouth, the so-called “dose- pacs,” because it requires very high doses to get enough steroids to the area of the irritated nerve to be effective. The high doses of oral steroids required to be effective can cause some rare but harmful side effects, such as an increase in blood sugar (diabetes), loss of bone mass (osteoporosis), bleeding ulcer in your stomach, and destruction of the hip joint (aseptic necrosis of the hip). These bad side effects from steroids taken by mouth are not as common when they are given by epidural injection.
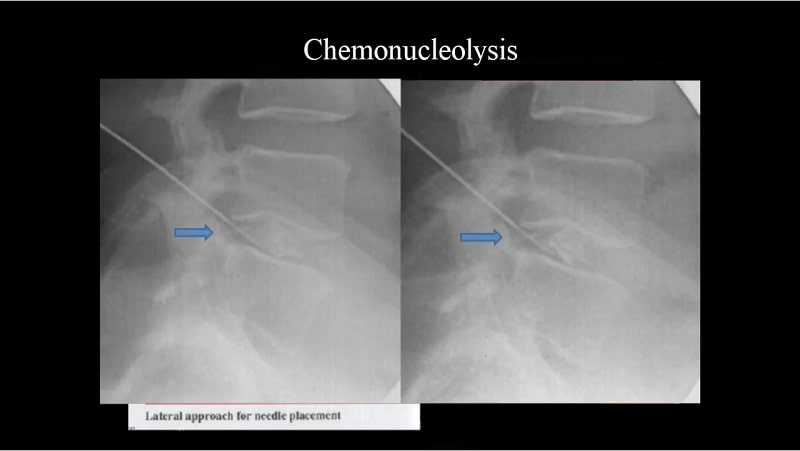
A specialist should perform the epidural injection using fluoroscopy (moving x-ray picture) to accurately place the steroid in the exact region of the painful nerve. I refer my patients to another specialist (anesthesiologist or physiatrist) to perform epidural injections. Your doctor may perform the epidural or may refer you to another specialist to have it performed.
What should I expect when I have an epidural?
First, a disclaimer: Unlike an MRI scan, I have personally never had an epidural, therefore I am relating to you what patients have told me about their experience with the procedure. Most patients say that it is not a very painful procedure, but a few patients do complain of experiencing a temporary increase in pain at the time of the injection. This is particularly true when the steroid is injected into the area of an irritated nerve. You can request sedation when it is being performed, but some patients do not want it. The injection includes a local anesthetic along with the steroid medication, which should give you some immediate pain relief. Immediate pain relief from the local anesthetic is an indication that the correct area was injected. I write a prescription stating the exact level and side of the herniated disc so that the doctor who is performing the procedure will know exactly where I want the injection to be placed. Accurate placement of the steroid is confirmed when the patient has immediate relief of pain from the local anesthetic in the injection. Immediate relief of your pain at the time of the epidural injection also helps to confirm the diagnosis that the disc herniation seen on your MRI scan is the actual cause of your pain.
Mark D. Brown is Professor and Chairman Emeritus of the Deparment of Orthopaedics and Rehabilitation, University of Miami Miller School of Medicine.