Back Surgery for Arthritis

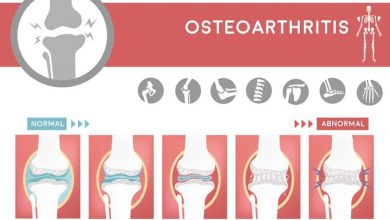
Arthritic changes in the spine can cause serious disability and pain and for many patients the symptoms become unmanageable using medications or conventional treatments, therefore many consider back surgery for arthritis. Where degeneration of spinal structures has led to compression of the spinal cord or stenosis which may result in permanent nerve damage the usual treatment is surgery to decompress and stabilize the spine. There are numerous types of back surgery and the appropriate treatment is not always immediately obvious. A patient will need to have diagnostic scans performed in order to assess the location of the nerve or cord compression and this may then be confirmed using selective nerve root blocks to ensure that the correct vertebral level is operated on. Misdiagnosis is the most common reason for failed back surgery syndrome as the real cause of the patients’ back pain has not been addressed in such circumstances.
Back Surgery for Arthritis
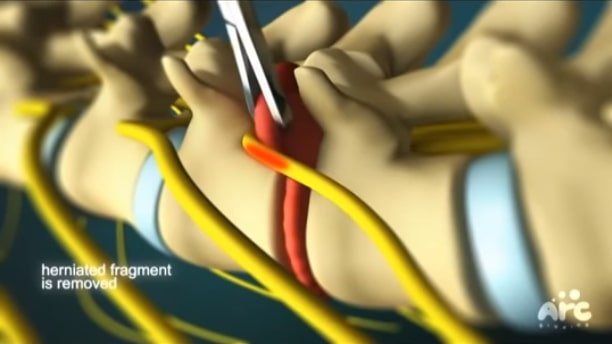
Back surgery for arthritis of the spine may involve removal of discs which have degenerated due to the condition and which are compressing the nerves or spinal cord. A discectomy is performed to remove either part or the whole of the disc at one or more levels. Where a small amount of the disc is removed this may be possible through a microforaminotomy, with minimal trauma inflicted on surrounding tissues and a subsequent short recovery time and low risk of complication. A microforaminotomy may also be helpful if the arthritis has resulted in bone spurs growing in the foramina themselves with significant nerve decompression occurring after these bony growth are removed.
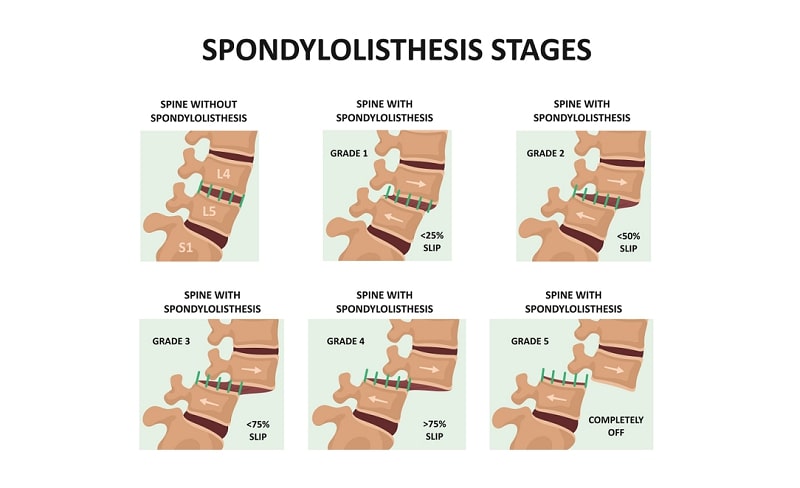
In many cases of arthritis however, the extent of the damage is more widespread and several vertebral levels will require intervention. It may be necessary, therefore, to remove the lamina at the back of the spine to decompress the entire spinal canal and provide better surgical access to the vertebra and facet joints. Bone spurs (osteophtyes) that have formed as an attempt by the spine to stabilize itself will be removed during such surgery and the spine will usually be fused using a bone graft in order to maintain its stability after the removal of structural tissue. Without spinal fusion after multiple level decompression back surgery the patient is likely to suffer from a loss of intervertebral height, spinal slippage (spondylolisthesis), and further nerve compression. With spinal fusion however, there is the possibility of adjacent segment syndrome where the vertebra above and below the area of operation are put under increased stress due to a redistribution of load-bearing responsibility in the spine.
Back Surgery can Exacerbate Arthritis Symptoms
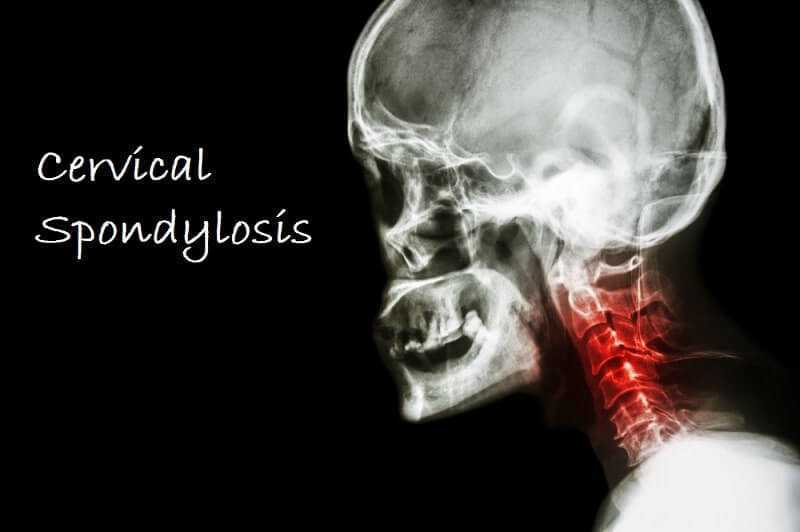
Problems with hypermobility in the spine may occur where muscles have become weaker or ligaments have been compromised or cut by previous trauma or back surgery. Stretching and strengthening exercises for the spine are important in order to reduce the risks of further degeneration. As the neck is more mobile than other areas of the spine it is the cervical spine which tends to suffer most due to wear and tear. Arthritis in the neck is a common condition resulting in pain and discomfort in the neck, back and shoulders. The lumbar spine may also be affected and back surgery for arthritis such as a transforaminal lumbar interbody fusion (TLIF) may help to stabilize the spine and reduce pain due to nerve compression and hypermobility. Fortunately, adjacent segment syndrome is less likely to occur in the lower lumbar spine than in the cervical spine, or upper sections of the lumbar spine, due to the relative lack of motion of these lower vertebral sections. In a small number of cases the symptoms of spinal arthritis are attributable to a thickening and hardening of the ligaments in the spine which then cause nerve and cord compression. Removing or severing these ligaments can help decompress the spine but may then cause hypermobility and an increased progression of degeneration in the facet joints and discs.

When is Back Surgery Appropriate for Arthritis?
Spondylosis (arthritis in the spine) itself increases the risks of other spinal problems as structural changes occur in the spinal column but it can also be a result of other spinal conditions such as acute trauma, disc herniation, whiplash, and musculoskeletal disease. Patients with other conditions affecting their thyroid, adrenal, or immune systems may experience spinal arthritis differently to otherwise healthy individuals as pain and inflammation can be exaggerated by their other issues. Similarly, rheumatoid arthritis in the spine can be both a cause of osteoarthritis symptoms and be accentuated by the presence of spinal degeneration due to wear and tear. Separating the causes and symptoms may not be easy, or possible in some cases, making the treatment of such conditions difficult.
Typical Treatment Plans
Most patients with arthritis will be given conservative treatment for at least six months prior to back surgery for arthritis being suggested and many do well on such a treatment plan. For others the ongoing pain and increased disability of spinal arthritis necessitates surgical intervention and may allow their symptoms to be relieved to some degree, although often these return due to the nature of the degenerative disease. Smokers are at a higher risk of degenerative spine problems and are also less likely to have favorable outcomes after surgery making it essential for anyone with back pain and arthritis to quit smoking prior to back surgery.





i have severe back arthritis. i am in severe pain and walk very slow. how can you help me