What Tests Can I Do?

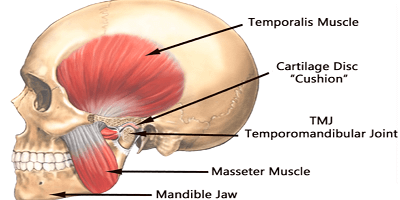
1. FEEL YOUR TMJ JOINT
The first test is simply to feel your temporomandibular joint, which is located about one finger’s width in front of your ear canal. Press, while slowly opening and closing, and feel if it is painful. Pain indicates something is wrong — either swelling or inflammation. Normal joints should not be painful. Press on your elbow or wrist and move it to compare how a joint should feel.
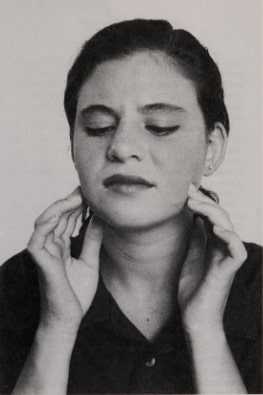
2. PRESS ON YOUR JAW MUSCLES
The second test is to feel your muscles. Normal muscles should not be painful or sore. Feel, or press, all of your facial and neck muscles for any areas of soreness or tenderness. Try rubbing the muscles on the lower border of your lower jaw. Clench your teeth and feel this muscle bulge. Then press and rub it to see if it is sore. Next, clench your teeth while placing your fingers on your temples and feel the muscle there bulge. Rub and press it to feel for soreness. Feel the muscles in the front of your neck, the back of your neck, and the back of your head and shoulders for soreness or sore spots.
Soreness indicates something is wrong with the muscle. Most of us have experienced sore muscles when we exercise too much. For example, if you go out running when your body is not used to the exercise, your leg muscles will be sore. Similarly, if you do a lot of lifting and you’re not used to it, you may find that your back muscles or shoulder muscles are sore.

Muscles also get sore when something is wrong with the joint in order to protect the joint. Muscles also can refer pain to other areas away from the muscle.
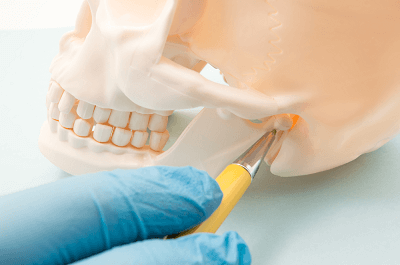
3. WATCH YOUR JAW OPEN
The third test for a TMJ problem is to check the movements of your jaw in front of a mirror. First, open your jaw slowly and see if it opens in a straight line or does your jaw deflect to one side or the other? How far can you open your jaw? Can you get at least two and a half fingers between your upper and lower teeth? Does your jaw move the same distance to the right and to the left? If any of these movements are not normal, there could be something wrong with your jaw or your TMJ joint.
4. LISTEN FOR NOISE
Another test is to listen for noises in your joint when you open and close your mouth. Does your joint pop, click, or make grating sounds? Be aware of these sounds
5. CHECK FOR PAIN
You should also observe for pain in your jaw joint or muscles. Does your jaw joint hurt when you chew food? Do you wake up with a sore jaw joint or sore muscles in the morning?
The purpose of these tests is to see if something is not working right. If you have pain or if you cannot properly use your jaw, then you need to have your physician or your dentist examine the problem.
What Other Medical Problems can be Confused with TMJ Problems?
Not all pain in the area of your jaws is caused by problems with the TMJ. Many other problems can mimic the symptoms of TMJ disorders.
Headaches
The typical TMJ headache is a pain located on the side of the face in front of the ear with the pain radiating back to the ear, up to the side of the nose and eye, and up onto the temple. Often the TMJ headache is accompanied by dizziness, loss of equilibrium, ringing in the ears, nausea and sensitivity to light. Headaches are very often one of the symptoms of TMJ disorders, but most headache sufferers do not have a TMJ disorder. At most, ten percent of all headaches are from TMJ disorders. There are many different types of headaches, and most of them have nothing to do with TMJ disorders. Headaches affect millions of people regularly, and it is rare to find someone who has never had a headache. Headaches have many different causes.

Migraine
A migraine is a vascular headache characterized by a preheadache phase that starts about 30 minutes before the actual headache. During this phase there often are visual symptoms ranging from blurriness to partial blindness. Other symptoms may be weakness, dizziness, mental confusion, or even tingling of the feet. Usually these symptoms diminish within 30 minutes and the headache begins, usually on one side of the head. Nausea, vomiting, achiness, and chills often accompany the headache.
Sinus Headache
A sinus headache results from a clogged sinus or an infection of the lining of the sinus. Allergies, most commonly hay fever, can irritate the sinus and cause a headache. Sinus headaches are often associated with colds or flu.
Muscle Contraction Headache
Muscle contraction headache, or tension headache, is the most common type of headache. It is also called a stress headache. It is often described as a tight, viselike band squeezing the head. It usually causes a constant dull ache that can last from hours to days. This type of headache is often associated with TMJ disorders.
Headaches As Symptoms of Other Medical Conditions
Many medical conditions can cause headaches. Infections, flus, colds, meningitis, head injury, brain tumor, stroke, and high blood pressure are examples. Toothaches can refer pain to the head and are a cause of headaches. Eyestrain, which can be caused by prolonged reading in poor light, can be the source of headaches.
Chemical Headaches
Many chemicals can cause headaches. Probably the best known is the hangover headache caused by alcohol. Other chemicals that can cause headaches are monosodium glutamate (MSG), nitrites (used as food preservatives in bacon and hot dogs), gasoline fumes, paint, paint thinner, glues, and turpentine. Carbon monoxide gas from car exhaust fumes can also cause headaches.
Ear Infection
Probably the disease that most often is confused with TMJ problems is an ear infection. Middle-ear infections are usually seen in young children but occasionally can occur in adults. These infections can cause severe earaches that can be confused with TMJ aches. Usually otitis media, or middle-ear infection, is associated with a fever.

More common in adults is otitis externa, often referred to as swimmer’s ear. If the ear canal is the site of an infection, the ear and area of the joint become very painful. Pressure on the TMJ can cause pain in this condition. Visual examination by a doctor will usually reveal an infected ear canal.
Sinusitis
Sinusitis can also be confused with temporomandibular joint pain. In sinusitis, the membranes lining the sinuses become inflamed, causing pain that is often felt in the upper teeth and can be referred to the temporomandibular joint.
Temporal Arteritis
Pain from arteries or blood vessels is another source of pain often confused with TMJ pain. One disorder of this type is called temporal arteritis. It is an inflammation of the temporal artery. The patient usually feels a sharp, diffuse pain in front of the ear, and pain can be referred up into the temple area. The pain comes suddenly and lasts for only a short time but returns again and again. Temporal arteritis if left untreated can lead to blindness.
Carotidynia
Another disease of vascular pain is called carotidynia. It causes an intermittent and aching pain over one temporomandibular joint and can radiate up into the temple area and into the ear. In this disease the external carotid artery, which is located in the side of the neck, becomes tender and swollen. Pressure on the artery makes the areas of the face and neck hurt.
Neuralgias
Neuralgias, or nerve pain, can also be confused with temporomandibular joint pain. Even though neuralgias usually cause sharp, severe, stabbing pain, they can at times be confused with temporomandibular joint pain. They can be set off by movement of the jaw, by swallowing, or by touching or moving a specific area. Usually they are differentiated from TMJ pain in that the pain is very severe and lasts for only a very short time.
LYME DISEASE
Bitten by a Tick
Heather complained of pain in her right temporomandibular joint and an inability to open her mouth more than one and a half fingers’ width. She also complained of pain in the joints of her knees and shoulders. She had a red rash on her legs that she had said had increased in size over the past week. When further questioned, Heather remembered that she had been bitten by a tick three weeks earlier. She had noticed a red rash around the area where she was bitten. It turned out that Heather had Lyme disease, which is caused by infection from bacteria that are carried in ticks and can cause rashes and pain in various joints of the body. Lyme disease can be treated with antibiotics, as was Heather, and the symptoms promptly disappear.
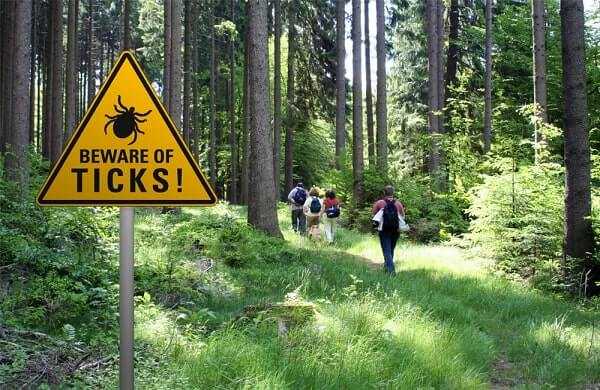


Lyme disease is becoming increasingly common in the United States. It is caused by a bacteria carried in ticks. Symptoms include headaches, stiff neck, chills, fever, muscle aches, marked fatigue, nausea, vomiting, skin rashes, and joint pains in various joints of the body, including the temporomandibular joint. A skin rash is seen near the site of the tick bite, and within three or four weeks the rash increases in size. The episodes of the joint pain usually last only about a week at a time. Treatment is with antibiotics, either penicillin or tetracycline. Usually after taking antibiotics for ten to twenty days, the symptoms disappear.
Related Article
Could Your Chronic Pain Be From Lyme Disease?
Arthritis
Arthritis, which is an inflammation of a joint, can attack the joints in the neck bones as well as the temporomandibular joint. It can also then cause the muscles that control those joints to become painful in order to protect the joint. There are several types of arthritis.
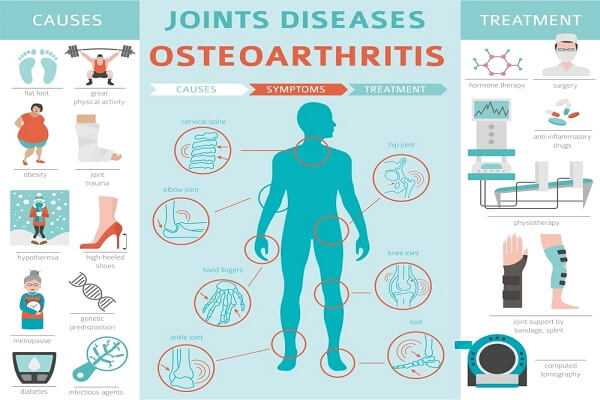
Osteoarthritis
Osteoarthritis, or degenerative arthritis, is the most common form of arthritis, and it can cause pain on movement of the joints. It is thought that it exists in almost every person in some joint after the age of 25 or 30. It is probably the result of years of wear and tear on the joints. The older one gets, the more evidence there is of osteoarthritis. Trauma to a joint increases the likelihood of osteoarthritis in the future. Osteoarthritis is probably responsible for many of the problems that we associate with aging, because, as people age, their joints become worn and rough and less able to move smoothly and bear up under heavy loads and stress. It is probably one of the reasons that most athletes retire after age 40.
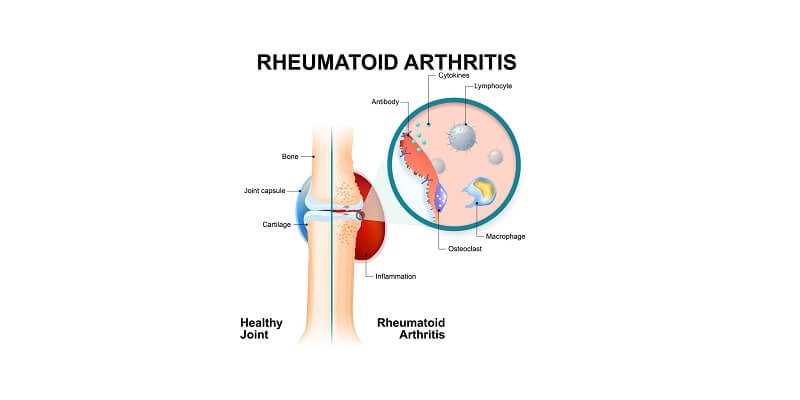
Rheumatoid Arthritis
Rheumatoid arthritis is much rarer than osteoarthritis, but it affects approximately 7 million people in the United States. It usually starts after 40. Rheumatoid arthritis is a type of auto-immune disease. It is a breakdown of the body’s immune response system. There is some evidence that it is associated with emotional trauma in some cases. Rheumatoid arthritis usually involves both sides of the body, that is, if it affects the hand and wrist, it’s usually both right and left. If it’s the knee, it’s both knees, and if it’s the TMJ, it’s usually both of them. It can cause the joints to become red, swollen, and painful. Rheumatoid arthritis usually should be managed by a physician. There are specialists called rheumatologists who specialize in managing this type of arthritis.
Other Types of Arthritis
Osteoarthritis and rheumatoid arthritis are the two major types of arthritis, but there are several other, rarer forms. Gout, juvenile rheumatoid arthritis, ankylosing spondylitis, arthritis from gonorrhea infection, psoriatic arthritis, and Reiters syndrome are other types of arthritis that have been known to affect the TMJ. These types of arthritis are fairly rare, especially in the area of the TMJ. There are many laboratory tests that your physician can perform in order to help diagnose the various types of arthritis.