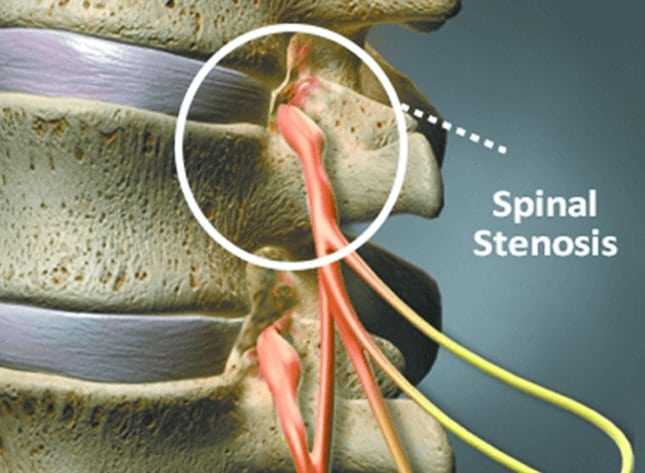
Spinal Stenosis Surgery – Things You Should Consider
As with any surgical procedure, undergoing spinal stenosis surgery is a significant decision to make. You may have been suffering from the symptoms associated with the condition – typically pain, numbness, weakness, and tingling that can affect the upper or lower body – for weeks or months, and the idea of surgery may seem like your only hope left to relieve your discomfort. If your doctor has suggested elective surgical intervention, it’s likely you are one of few patients for whom surgery is, in fact, a final treatment option. That said, it’s important that you carefully weigh all of the advantages and disadvantages associated with spinal stenosis surgery before you sign any consent forms.
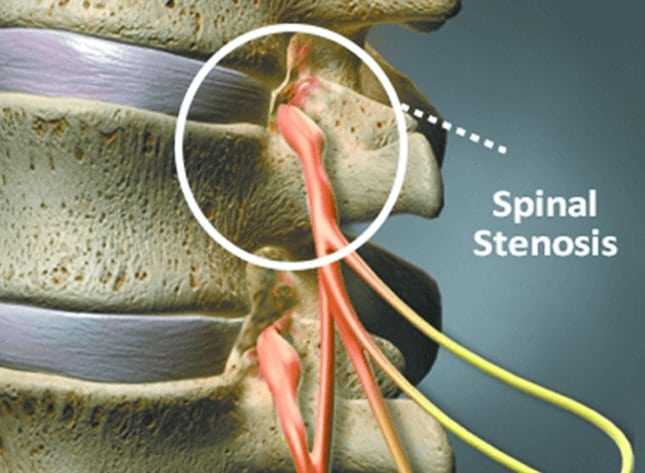
Open Spine vs. Minimally Invasive
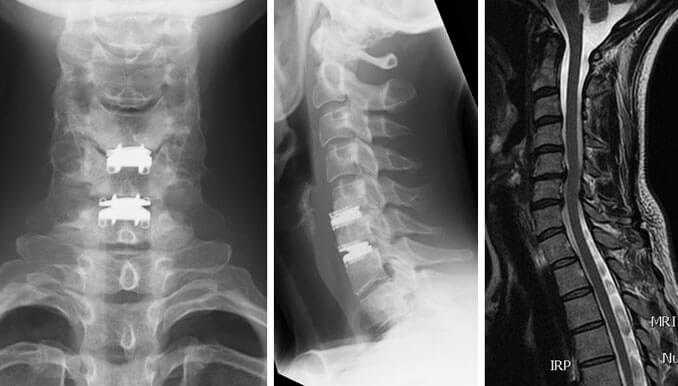
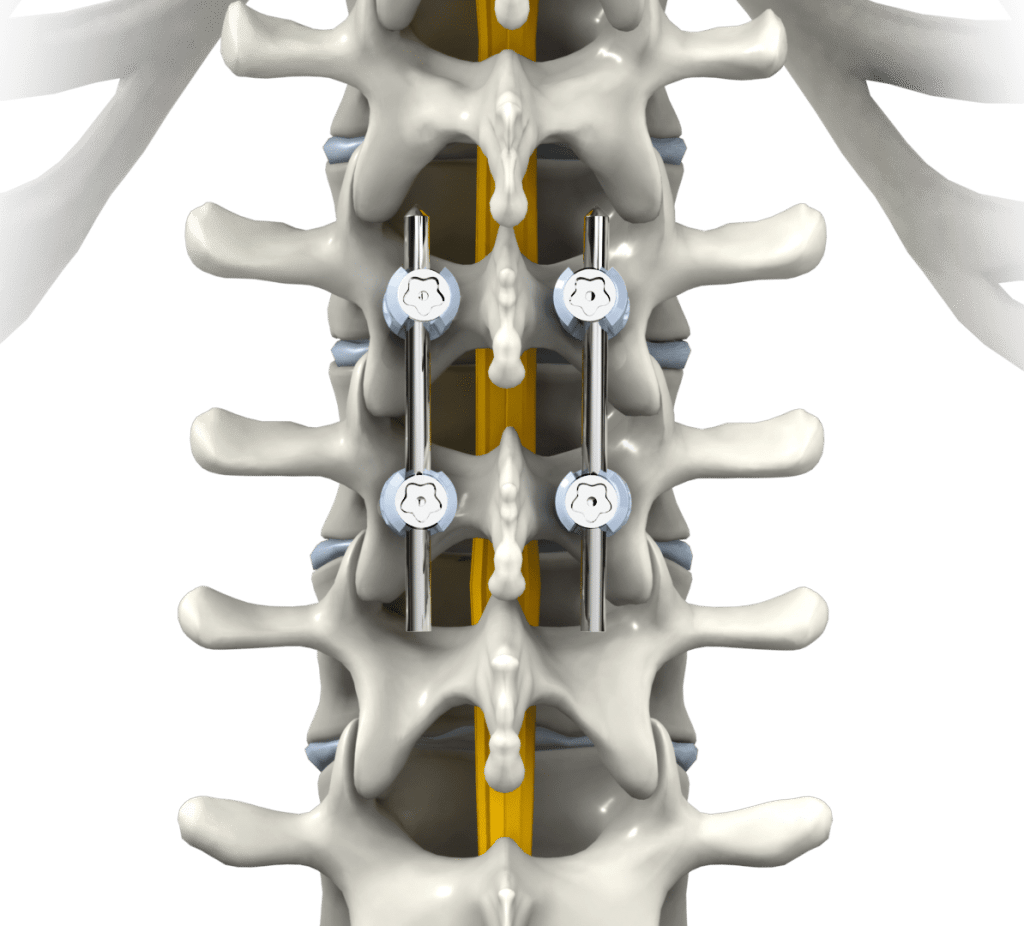
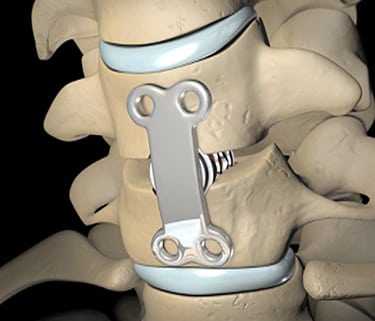
Depending on your unique condition, age, and overall health, your doctor will suggest one of two approaches to spinal stenosis surgery to decompress your spinal cord or a nerve root affected by the narrowing (“stenosis”) of the spinal canal or a foramen. The first approach, open spine surgery, is a highly invasive option that requires a large incision in the neck or back, muscle dissection, and the removal of a large amount of spinal anatomy. This type of surgery can affect the stability of the spine overall, so spinal fusion, or the permanent affixing of two individual vertebrae with screws, rods, and bone grafts, may also be performed. As a highly invasive operation, open spine surgery carries with it elevated risks of bleeding, infection, nerve damage, and an extended recovery period, as well as the possibility for the development of new or worsened symptoms.
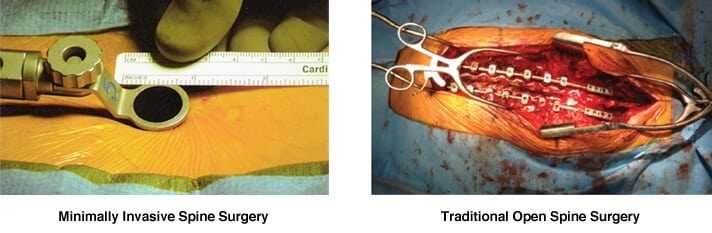
Minimally invasive spinal stenosis surgery, on the other hand, is a much less daunting surgical option. This type of procedure involves an endoscope, small surgical tools, and sometimes a laser, which are fed through telescoping tubes inserted into a small incision near the affected area of the spine. Musculature and surrounding soft tissues are left relatively undisturbed, and only minimal disc material, ligamentous tissue, or bone material are removed, leaving the spinal anatomy largely intact. As a result, risks factors like bleeding and infection are reduced, and the recovery period is usually much faster than that of open spine surgery
Check with Your Doctor
If you feel confused about which spinal stenosis surgery option you should choose, consult your doctor. He or she can help you consider factors like your occupation, lifestyle, and activity level to help you decide. It should be noted that not every spinal stenosis patient is a candidate for a minimally invasive procedure, so be sure to thoroughly discuss this surgical option with your doctor and consider looking into additional medical opinions.
Understanding Your Surgical Options
If your doctor has asked you to consider undergoing a spinal stenosis procedure, you are one of many individuals suffering from the persistent symptoms of spinal canal and/or foraminal canal narrowing. Your symptoms have probably been unresponsive to conservative treatments, and as a result, your doctor believes that you require surgery to decompress your spinal cord or a nerve root. Before you agree to any procedure, it’s in your best interest to learn as much as you can about the surgical options available to you.
Open Spine Surgeries Used to Be the Norm
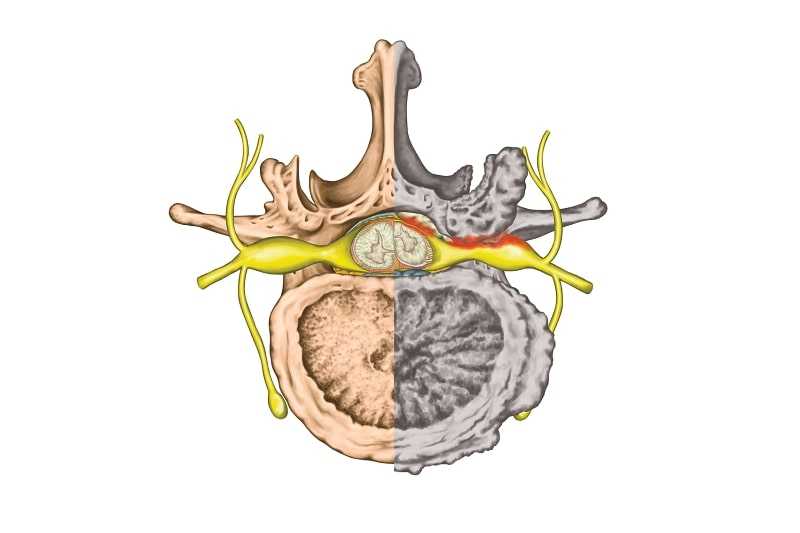
Not too long ago, the only surgical option for a decompression spinal stenosis procedure was open back or neck surgery. Still used today, these types of operations require a large incision in the neck, back, side of the torso, or abdomen. Muscles and other soft tissues are dissected so a surgeon can access the affected area of the spine. Spinal stenosis usually involves a bulging or herniated disc, thickened ligament, vertebral slippage, or some other abnormality invading the spinal canal and/or foraminal canal space and compressing the spinal cord or a nerve root. During an open spine surgery, a surgeon will remove whatever soft tissue or bone material is necessary to open up space in the spinal column and decompress the nerve. Sometimes, a large amount of spinal anatomy is removed, rendering the spine unstable. In these instances, a spinal fusion may also be performed, involving support cages, rods, screws, and bone grafts to effectively and permanently fuse two vertebrae together and halt movement in that segment. Open spine surgery is highly invasive and may lead to a lengthy, painful recovery. You may, however, be a candidate for a minimally invasive alternative.
Minimally Invasive Procedures are Now Available
Thanks to advances in technology and science, some surgeons are now able to perform a spinal stenosis procedure with a minimally invasive approach. These types of procedures involve an endoscope, or camera, that is inserted into a small incision near the compressed neural structure. Tiny surgical tools and a laser are also inserted, and are used to cut away or vaporize the bone material or soft tissue causing compression. Since the back or neck musculature remains relatively undisturbed, a minimally invasive procedure typically allows for a faster recovery than the recovery period after open spine surgery.
You should understand all of the benefits and risks associated with your chosen spinal stenosis procedure. Consult your doctor or a spine specialist to find out which surgical approach is right for you.

for more detailed information about spinal stenosis