Spinal Fusion for Degenerative Disc Disease (DDD)
Second only to the controversy surrounding the diagnosis of degenerative disc disease (DDD) as a cause of low back pain is that concerning surgery for this condition. Of the 10% of patients with acute back pain who develop chronicity, about 40% are found to have DDD as evidenced by examination, MRI, and discography. Of these about 30% do not respond to conservative measures. That leaves about 1 in 100 individuals in this age group who develop acute back pain as eventually being a candidate for surgical fusion. With a population of 15 million adults in the age bracket 20-50 in Canada, for example, and an incidence of acute back pain of 50%, that makes about 90,000 patients per year eligible for surgical consideration! This figure is both impractical and improbable. A marked reduction in this number results from both patients unwilling to consider surgery and patients not suitable for any number of reasons.
Indications for surgery include chronic, disabling back pain unresponsive to an adequate trial of conservative treatment. There should be no evidence of disc herniation, and positive degenerative MRI findings should correlate with discographic symptoms and the overall clinical picture. In addition, there should be no underlying significant psychological factors because these should definitely be addressed prior to any surgical intervention. Of course, these indications are only guidelines, and each case should be taken on its individual merits.
Procedure
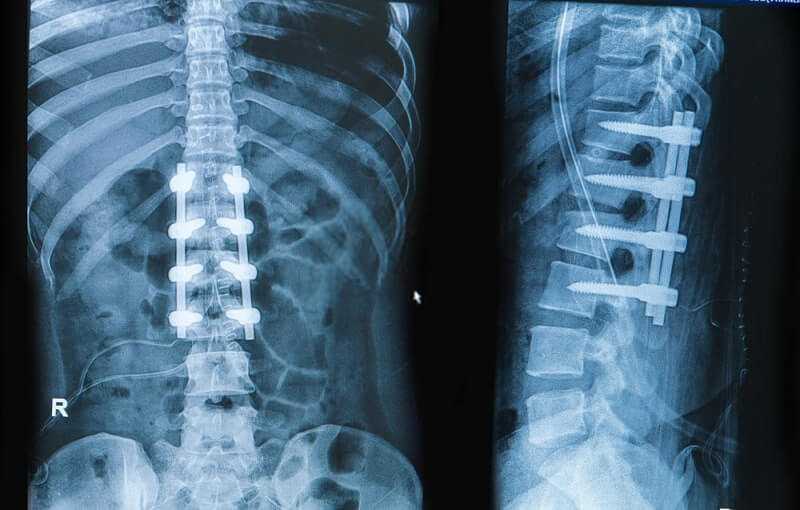
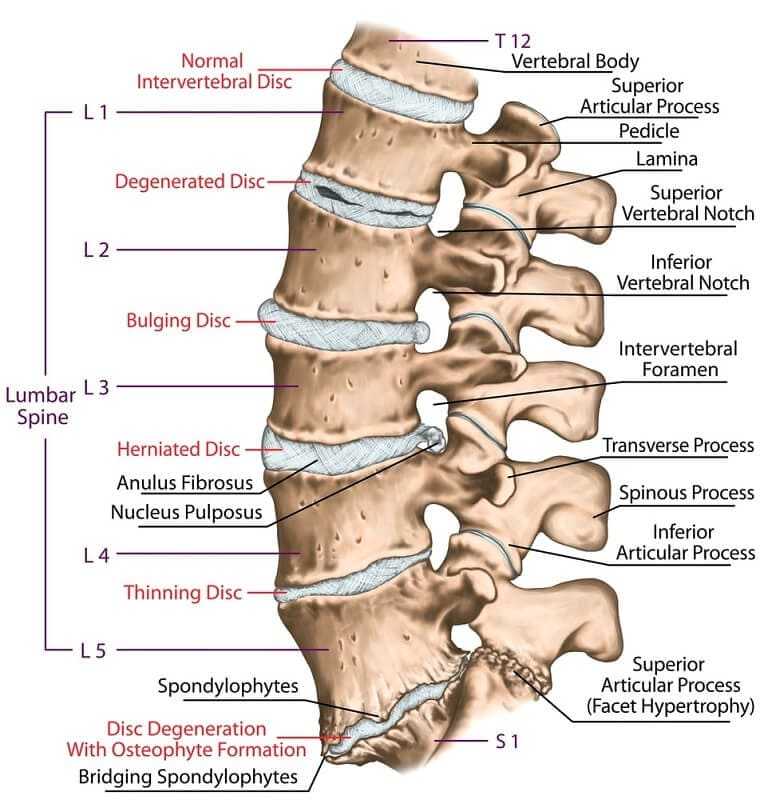
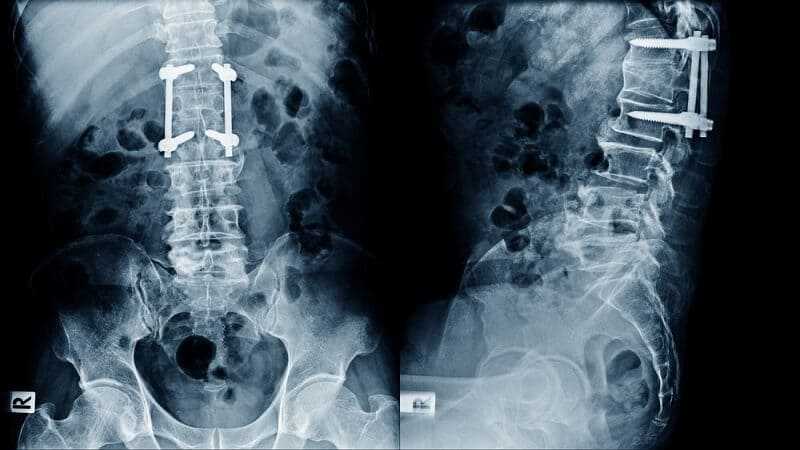
The most common procedure for fusion in DDD is posterolateral decortication (removal of hard surface bone to expose soft inner spongy bone) and bone grafting with or without metal instrumentation. This is similar to the technique described above for ‘decompression with fusion’, although in this case the decompression is not generally required. Newer techniques approach the fusion from the front of the spine via the abdomen and may use open surgical exposure or laparoscopy (small incisions with fiber-optic visualization). These so-called ‘anterior interbody fusions’ often employ metallic hardware or ‘cages’ filled with bone graft to achieve fusion.
https://www.youtube.com/watch?v=hnSFcHX21Pshttps://www.youtube.com/watch?v=37UqKwdGFX4
Results
Although the techniques to achieve fusion have improved and have become extremely reliable, we have not been able to demonstrate a reliable reduction in low back pain with this procedure. A study in 2000 found no clear scientific evidence to support decompression or fusion for treatment of DDD. Individual studies, however, have found it to benefit a high proportion (nearly 90%) of carefully selected patients; it is likely that this selection process is the key. For example, fusion is a very useful option for individuals with isolated, severe degenerative changes at L5/S1 and with the remainder of the spine looking quite healthy.
Although between 55% and 90% of individuals report initial relief of symptoms, recent literature indicates that this number may deteriorate over the course of a few years. Some may go on to develop degenerative changes at adjacent levels. Whether or not this is secondary to the fusion itself, or merely a manifestation of the natural history of the disease process, is unknown. The relevance of this finding is also controversial. One paper compared patients who had spinal fusion for DDD to those who had other, non-fusion surgery. They found that 20 years later, although disc degeneration above and below the level of the fusion was twice as common in the fusion group on X-rays, there was no difference in clinical outcome.
Nevertheless, there is a role for spinal fusion in DDD. Research over the next few years should more clearly define its role and the specific group of patients it is likely to benefit.
Spinal Fusion for Degenerative Disc Disease (DDD) Facts
Ensuring the patient with Degenerative Disc Disease (DDD) is an optimum candidate for spinal fusion is essential in securing a successful outcome.
Indications
• Chronic or frequently recurrent, severe, disabling low back pain.
• Failure of at least 6 months adequate conservative therapy.
• Positive MR I findings.
• Positive discography at no more than 2 disc levels and correlation with MRI findings.
• No evidence of disc herniation, instability, or spinal stenosis.
• Correlation with clinical picture.
• Absence of significant psychological factors.
Factors that Impair Successful Fusion
• Smoking: healing is 3-4 times slower in smokers. • NSAIDs: avoid if possible as they impair bone healing. • Steroids: use reduces bone healing. • Nutrition: inadequate nutrition impairs healing.
Factors that Promote Successful Fusion
• Instrumentation: use of metal screws and rods promotes fusion
• Osteoinductive Proteins: newly isolated proteins added to bone graft improve healing.
• Gene Therapy: promising experimental studies.
• Electromagnetic Therapy: no conclusive evidence that it is beneficial.





