Back PainHerniated Disc
Acute Intervertebral Disc Herniation
Basics
Description
- Axial or radicular pain occurs following an acute injury to the intervertebral disc.
- May be due to trauma, lifting injuries, or idiopathic.
- Cervical, thoracic uncommon

Epidemiology
Incidence
National incidence of herniated nucleolus pulposus is 1.7%.
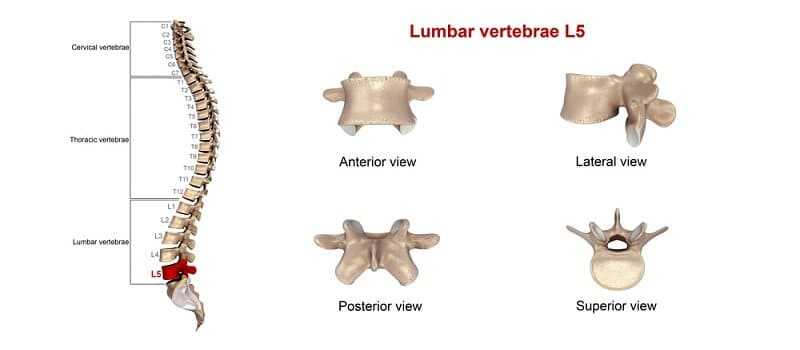
- Majority occur in lumbar region (95% L4–L5 or L5–S1).
- Second most common occur in cervical region (C5–C6, C6–C7 most common).
- Thoracic region accounts for only 0.15% to 4.0 % of cases.

Prevalence
Gender:
- 4.8% males older than 35 experience sciatica during their lifetime.
- 2.5% females older than 35 experience sciatica during their lifetime.
- Of all individuals, 60% to 80% experience back
pain during their lifetime.
- In 14%, pain lasts more than 2 weeks.
- Generally, males have a slightly higher incidence than females.
Risk Factors
Genetics
- Familial link to discogenic low back pain, no HLA correlation
- May be congenital link to herniation
- May be genetic link to disc degeneration in twins’ studies
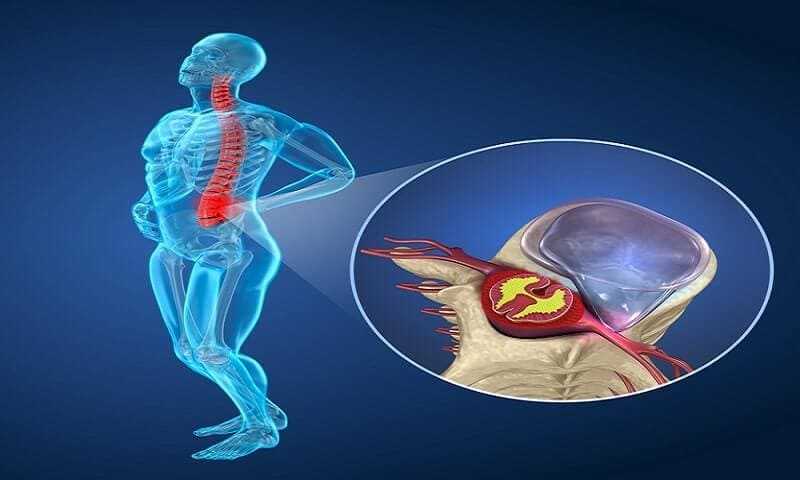
Pathophysiology
- By late 20s and early 30s, nucleus pulposus loses vascular supply and dehydration/degeneration begins.
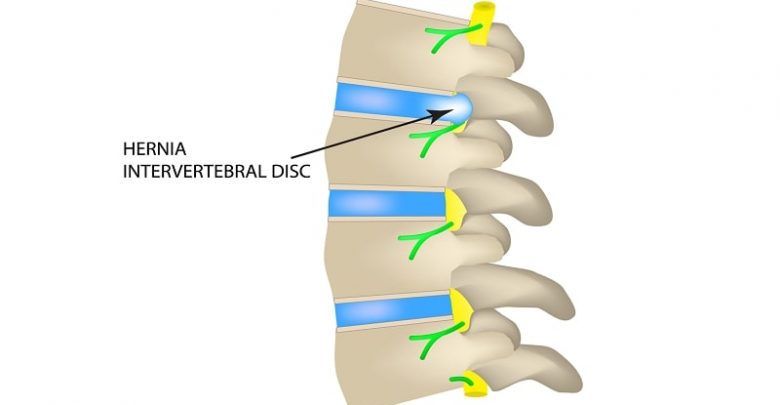
- Acute radiculopathy is caused by prolapse of a sequestered fragment of disc through a tear in the annulus fibrosis.
- Herniations, often posterolateral, incite intense irritation of nerve roots and increases in local inflammatory mediators such as proteinases, nitric acid, phospholipase A2, prostaglandin E2, and IL-6.
- Lateral (foraminal) herniations result primarily in nerve root compression and radicular symptoms.
- Dorsolateral herniations may compress the exiting nerve root and create a combination of radicular pain and motor weakness.
- Midline herniations produce primarily myelopathy.

Etiology
- Minor trauma, such as lifting, bending, twisting, and vigorous athletic maneuvers, are implicated.
- Major trauma, such as motor vehicle accidents, falls, and industrial accidents, may result in herniation, especially with vertebral fractures.
- Injury may result after no identifiable traumatic event.
- Often occurs in the early hours of the day, after extended periods in recumbent position while sleeping.
Diagnosis
Signs and Symptoms
History
- The history and differential diagnosis for a complaint of back pain and/or leg pain is complex.
- Generally, acute herniation is more common in younger populations.
- Patients may have a history of either back or neck pain with periodic exacerbations, or may have no history at all.
- A precipitating event or trauma often occurs, and the patient may develop symptoms immediately or gradually over several days.
- Some patients will report a “pop.”
- Complaints range from isolated back, thoracic, or neck pain, to very specific radicular pain in a single nerve root distribution. Pain often is described as sharp, shooting, or stinging. Knowledge of radiation patterns is critical to accurate assessment.
- Patients may complain of paresthesia and weakness. Symptoms often exacerbated by maneuvers that increase intraspinal or intradiscal pressure such as Valsalva, coughing, sneezing, and defecation.
- Pain often improves while supine or when activity decreases. Complaints of associated muscle spasm are common.
- Suspect cauda equina syndrome with complaint of progressive weakness, difficulty with urination, increased frequency, overflow incontinence, perianal numbness, saddle dysesthesia, and loss of rectal tone; these cases require immediate surgical referral.
Physical Exam
- Comprehensive musculoskeletal and neurologic exam is mandatory.
- In lumbar injuries, inspection and gait analysis may demonstrate affected leg in flexed position, with patient listing away from the side of the irritated nerve root.
- Antalgic gait, with quick transfer of weight away from affected side, is seen.
- Evidence of motor weakness can be seen.
- Marked reduction in range of motion is common in cervical and lumbar regions, with loss of lumbar lordosis due to spasm.
- Tenderness to palpation, hyperesthesia, tenseness is present.
- Muscular atrophy may be present.
- Positive straight leg raise for lumbar, radicular pain on cervical foraminal compression (Spurling sign) maneuvers seen.
- Neurologic examination demonstrates weakness or loss of sensation to cold and sharp stimulus in corresponding nerve root distributions.
Alert
Note: Nerve root involvement usually is seen below the level of herniation. Example: L4–L5 herniation affects L5 nerve root.

Interventional Diagnosis
Selective nerve root injection with local anesthetic may help establish diagnosis of radiculopathy in cases where history, imaging, and electrodiagnostic testing is unclear.
Tests
Imaging
- MRI with and without gadolinium contrast
- CT myelogram in patients with MRI contraindication
- Axial CT scan

Diagnostic Procedures/Surgery
EMG/nerve conduction studies for radiculopathy, minimum of 14 days after symptoms begin.
Differential Diagnosis
- Mechanical pain
- Discogenic pain
- Myofacial pain
- Spondylosis/spondylolisthesis
- Spinal stenosis
- Abscess
- Hematoma
- Discitis/osteomyelitis
- Mass lesion/malignancy Myocardial infarction
- Aortic dissection
Medication (Drugs)
First Line
- Nonsteroidal anti-inflammatories (NSAIDs)
- Acetaminophen
- Tramadol
- Mild opioids for short-term use only Muscle relaxants
Second Line
- Oral corticosteroid taper
- Gabapentin
- Tricyclic antidepressants
Interventional
- Epidural steroid injection if conservative measures fail
- Transforaminal epidural or selective nerve root injection(Spinal Injections For Back Pain)
Rehabilitation
- Education
- Short- and long-term goals set
- Posture mechanics
- Hamstring, quadriceps, hip flexors, and calf stretching Lumbar stabilization
- Abdominal strengthening/pelvic tilt
- Improve range of motion
- Superficial heat and ice
Mental Health/Behavioral
- Identification and treatment of cormorbid mood disorders
- Adjustment and adaptation to injury state, to reduce further injury and optimize activity status
- Education regarding appropriate pacing of activities and avoidance of prolonged rest
Surgery
Special Therapy
Complementary and Alternative Medicine
Follow-Up
Prognosis
- Generally good
- Worse prognosis if symptoms persist after conservative measures are employed
- Risk of permanent nerve injury if progressive weakness is not addressed surgically
Issues for Referral
Referral to pain physician or surgeon if conservative measures fail.
Complications
- Permanent nerve injury
- Cauda equina syndrome
- Paralysis
- Chronic pain